INTRODUCTION
The aseptic technique is a method of preventing the transmission of infection to the patient during the performance of various clinical procedures. The correct practice of this technique requires the understanding of some principles and facts.
BASIC FACTS RE: MICROORGANISMS & INFECTION
Microorganisms are everywhere in the environment. Since they cannot be seen with the naked eye their presence should be assumed. Infection is caused by microorganisms (Bacteria, fungi, protozoa & viruses). Some species consistently cause infection while others cause infection only in certain conditions and situations. Yet most microorganisms are quite harmless.
Infection is dependent on:
- Number of organisms
- Virulence of the organism
- Predisposition of host environment to infection
- Degree of resistance of the host
Organisms can be transferred (transmitted) from one location (animate and inanimate) to another through the air, via droplets, and, most importantly, through contact.Organisms can either be reduced in number by disinfection or removed entirely by various sterilization methods.
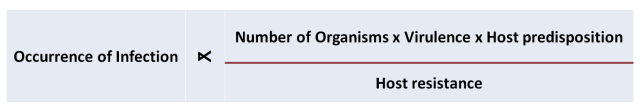
The interplay between the factors can be represented by the equation.
Factors Influencing Development of Infection
STRATEGIES IN PREVENTION OF INFECTION
During the performance of clinical procedures, the prevention of infection are be achieved through approaches based on the facts mentioned above. These approaches include:
- Minimizing the amount of microorganisms and dust in the environment through general cleanliness of rooms, air and equipment.
- Reduction of bacteria at the point of entry (skin or mucosa of patients) of the host through the use of antiseptics
- Reduction of bacteria on the care provider especially the hands through hand washing, gowning and wearing sterile gloves.
- Prevention of re-contamination of sterilized or disinfected instruments by avoiding contact between sterile and non-sterile items
- Reducing predisposition of host to infection by:
- minimizing tissue injury and ischaemia including excessive use of diathermy and sutures that are too tight
- reducing presence of blood clots
- shortening duration of retention of catheters / drains
- optimizing host resistance or immunity
A single breach of aseptic technique may introduce only a small quantity of microorganism and may not lead to a serious outcome because the small numbers may be taken care of by the host defense mechanism. However multiple breaches would result in a cumulative effect leading to the quantity of bacteria reaching a significant level for the development of infection.
The development of infection is also dependent on the type of organism.
Another factor is the immunity of the host. Immunocompromized (Neutropaenic) patients, babies, the elderly, diabetics and malnourished patients are especially at risk. Therefore, efforts must be made to reduce the breach of aseptic technique to the minimum.
INDICATIONS FOR ASEPTIC TECHNIQUE
Strict adherence to aseptic technique is indicated when performing invasive procedures including those:
Where a body canal or cavity normally free of microorganism (like trachea, bronchus, urethra, bladder, ureter, kidney pelvis and calices, uterine cavity, CSF and peritoneum), is entered (e.g. catheterisation, endoscopy, endoscopic surgery, insertion of intraperitoneal / Tenckhoff catheters)
When the skin or mucous membranes are breached (surgery, insertion of IV or Arterial lines, lumbar puncture, insertion of epidural catheters)
Managing traumatic and surgical wounds
Where a site already has resident bacteria (i.e. nose, external ear, throat, vagina), or is an infected wound; it is also important to follow (albeit a less strict) aseptic technique in order to prevent the introduction of other more virulent organisms especially the usual hospital resident species such as Multiresistant Staphlococcus aureus, Pseudomonas aerogenosa, Klebsiella pneumonia, Acinetobacter and Extended spectrum beta-lactamase producing organisms (ESBL)
PRINCIPLES OF THE ASEPTIC TECHNIQUE
The technique consists of the following set of processes:
- Creating a microorganism-free environment (sterile field)
- Use of sterilized instruments and dressings
- Maintaining sterility of sterile field and instruments by preventing microbial contaminationby contact with non-sterile objects; such as:
- the patient’s body,t
- he care providers body,
- non-sterile instruments,
- equipment,
- body fluids etc.
- Antisepsis of point of entry and hands of task performer.
CREATING A STERILE FIELD
The sterile field is a microorganism-free area without danger of them being contaminated. It is made up of two areas i.e.:
- The first area is a place that accommodates the instruments, dressing and lotions to place instruments used for the intended procedure. Usually, this is created by opening a sterile set fully on a trolley. The inside of the wrapper forms the sterile work surface. No other items should be on the trolley. It is important for this area is wide enough to accommodate all instruments.
- The second is a designated work area for the care provider to perform his/her tasks on the patient. It is created by covering the patient’s body and bed or table that he/she lies on with drapes made of sterilized fabric or synthetic sheets.
USE OF STERILIZED INSTRUMENTS AND DRESSINGS
Instruments used in invasive procedures are usually pre-sterilized. Sterilization removes all forms of microorganisms including spores.
Disposable instruments are sterilized using Ethylene oxide gas sterilization or Gamma radiation and kept sterile in packages. Reusable items are sterilized by steam at high temperature (autoclaving) or chemicals (Ethylene oxide etc.). Some instruments e.g. endoscopes cannot be sterilized by high temperature sterilization. Low temperature plasma sterilization technique (SterradTM) or high level disinfectant is then used. Proprietary dressings are usually sterilized by Gamma radiation whereas gauze is autoclaved at the hospital’s Central Sterile Supplies Department (CSSD).
Disinfection and Use of Endoscopes in Sterile Body Passages
Endoscopes passed into body cavities that do not have indigenous bacteria or are not colonized by bacteria, must be disinfected before use. These include bronchoscopes, cystoscopes, ureteroscopes, brposcopes and hysteroscopes. Disinfection removes all bacteria and viruses except spores. The instruments can be disinfected using chemicals such as glutaraldehyde (CidexTM), Gigasept and Peracetic acid. Disinfection should be done just before use and the instrument kept in a sterile field. It is not proper for these instruments to be disinfected a day onchoscopes or more earlier.
Instruments that become heavily contaminated must be sterilized. Chemical sterilization differs from disinfection in the duration of soaking i.e. at least 30 minutes or more for sterilization as opposed to 10 minutes for disinfection. Otherwise low temperature hydrogen peroxide plasma sterilization sterilizer (e.g. SterradTM) is used.
Biopsy forceps, catheters and stents must be sterile (preferably disposable).
Use of Speculum & Endoscopes in Non-Sterile Body Passages
Instruments and endoscopes passed into body cavities that has resident bacteria or are likely to be colonized by bacteria such as the mouth, vagina, nose, pharynx, external ear, esophagus, stomach, duodenum and colon, must be disinfected but not necessarily asterilized. They can be disinfected using disinfectants (glutaraldehyde [CidexTM], 70% Alcohol, Gigasept, Peracetic acid, Formaldehyde, Trigene, Sodium hypochlorite). Once disinfected, they can be kept in a clean environment. They should not be allowed to be re-contaminated e.g. by contact with an unwashed hand or dirty surfaces.
MAINTAINING STERILITY OF STERILE FIELD & INSTRUMENTS
Contamination of the sterile field will cause contamination of the instruments and other items within it. If only gloves are worn (no gowns) then the rest of the body should not come into contact with the sterile field. If the care provider wears a sterile gown, he/she is allowed to be in contact with the sterile field. Sterile instruments should not protrude out. Non-sterile items should not be allowed to enter the sterile field.
MINIMIZING BACTERIA AT ENTRY POINTS BY ANTISEPSIS
This depends on the site where the procedure is to be performed. The patient’s skin harbour commensals (e.g. Staphylococus epidermidis), which are harmless on the skin surface but may induce disease in the blood circulation or through it to distant sites like heart valves, the urinary tract, the biliary tract, the lungs or the brain. When patients are hospitalized, their skin may be colonized within a short time by bacteria of the hospital environment e.g. more virulent strains of Staphylococcus aureus. The patient’s skin can never be made sterile, but the amount of bacteria can be reduced by the use of antiseptics such as: Povidone iodine, 70% alcohol, Chlorhexidene 1:200 or mixtures of these.
Other surfaces including the mucosa of oral cavity, pharynx, nose, and vagina have different sets of resident bacteria and similar but appropriate antiseptics can be used.
PRACTICE OF ASEPTIC TECHNIQUE
MAINTAINING THE STERILITY OF INSTRUMENTS, DEVICES & SOLUTIONS DURING TRANSPORT AND STORAGE
The sterility of sterilized items are maintained by packing them in envelops, wrappers or containers. The items remain sterile if:
- the integrity of packages are maintained
- they are properly opened and introduced into the sterile field before use
- kept within the sterile field without being contaminated during use
During transfer and storage sterility may be lost if:
- the packages are punctured,
- liquid has seeped through the package
- the packages are accidentally opened
Such items should not be used. They should be re-sterilized if possible.
During transport, proper trolleys and containers should be used. Storage areas should be kept clean, free of vermin and away from water sprays.
Antiseptic solutions, including saline, should be of adequate strength and not diluted (e.g. Chlorohexidine 1: 2000 is ineffective). They need to have a ‘use by’ date. ‘In use’ test (C&S) need to be done now and then.
NON-TOUCH TECHNIQUE
Microorganisms especially bacteria is everywhere in the environment. Their content in the air is dependent on:
- the cleanliness of the room and equipment within it
- filtration of the air
- air exchange (removal of stale air in exchange for fresh air)
- direction of flow (from clean to non-clean areas)
These facts and that the bacteria can be killed by heat was known to Louis Pasteur 1887 Ref: http://en.wikipedia.org/wiki/Louis_Pasteur
In most clinical settings the amount and type of organisms in the air is minimal. As such, exposure of objects to air for the duration of clinical procedures is not considered as contamination and does not cause them to loose their sterility.
However, contact with any other non-sterilized object renders the instrument or item non-sterile. Hence the most effective way of maintaining sterility of sterilized instruments and other items is the non-touch technique. In this technique work processes are devised so that the sterile or disinfected item or instrument does not come into contact with non-sterile items. This can be achieved by studying the possible instances where contamination can occur in the context of various procedures and devising methods of avoiding it.
The non-touch technique ensures that instruments or items remain sterile during a procedure. When opening packets / envelopes ensure that the inside of the packet is not touched. Transfer the item or the inside package from the packet to the sterile field by either dropping it in, grasping it with a gloved hand / sterile forceps without touching the exterior of the packet. The entire sterile instruments / disposable items (such as lines and catheters) should lie within a sterile field.
If a non-sterile instrument is to be used during the procedure, then sterile sleeves or sterile see through covers need to be used (ultrasound probes microscopes, button & switches).
MAINTAINING STERILITY OF THE GLOVED HAND
Sterile gloves are worn to render the hand sterile since washing hands with antiseptic alone will only reduce the number of bacteria on it. Hand washing is still an essential part of aseptic technique because gloves may have inherent holes or become perforated during the procedure.
Therefore, hand washing according to the accepted procedure is mandatory especially when performing surgery. For the first case for the day, scrub the nails and fingers with a soft brush until clean. Wash hands until the elbow, preferably with Propyl alcohol plus Chlorohexidine mixture or Povidone iodine, for 5 minutes. For the subsequent cases a 2-3 minute hand wash until the elbow is sufficient. There is no need to scrub the forearms.
In practice it is very easy for the gloved hand to be re-contaminated unless strict precautions are taken. Some of these include:
- During the gloving process, touch only the inside of the glove with the non-gloved washed hand. The outside of the glove can be touched with the gloved hand.
- Once gloved, do not touch non-sterile areas or articles with the gloved hand. Remember that the patient’s skin is non-sterile. Surgeons should not poke their finger into the lumen of intestines! If there is a need to do so, the glove should be changed immediately.
- If the glove is punctured torn or contaminated, replace it.
ASEPTIC TECHNIQUE IN VARIOUS SITUATIONS
PROCEDURE WHEN WORKING ALONE
When working alone, perform tasks that do not require a sterile hand first before gloving. For example, when preparing sets / instruments for a procedure open the set, create the sterile field and put in additional items or lotions first. Open the outer envelope of the gloves packet fully before washing the hand.
When one hand is required to perform a task requiring contact with a non-sterile object or surface, consciously identify the contaminated hand and perform procedures with the other hand. The common situations include:
Performing Urinary Catheterization
Hold the labia minora apart or slide back the prepuce of penis with the non-dominant hand (usually left). Cleanse the urethral opening with antiseptic and insert the catheter with the dominant sterile hand.
Performing Laryngeal Suction on a Patient with Tracheostomy
Hold the non-sterile sucker tubing with the left hand and the sterile suction catheter with the right hand.
Disconnecting & Reconnecting IV/Arterial cannulas
Contamination of cannulas and lines can lead to line sepsis. This is unlikely if cannulas are retained for short periods (not > 48 hours). However central lines, femoral lines and umbilical artery & vein catheters pose a higher risk which in turn may cause systemic sepsis or infection at distant sites. In neonates, a possible distressing complication is septic arthritis and osteomyelitis at the metaphyses.
The connector takes the form of a Luer lock with the tip of the line being male while the flange of the cannula is female. The inside of the tip of the line must be kept sterile. The entire flange of the cannula should remain sterile.
To disconnect, grasp the base of the cannula firmly, occlude the vein or artery with a finger and untwist the tip of the line with the other hand. The tip must then be kept sterile by holding it in the air by hanging on the drip stand with the help of a pre-prepared tape or by asking the patient to hold the line a short distance from the tip. Place a spigot or stopper into the flange of the cannula. A sheathed needle or spigot is then used to occlude and cover the tip of the infusion line.
To reconnect, remove the needle or spigot from the line tip. Then hold the base of the cannula firmly and remove the spigot or stopper. Twist back the tip of the line into the flange of the cannula.
In fact, it is quite difficult to prevent contamination during this procedure when performed by a single individual. It is better if it is performed by two persons.
PROCEDURES WHERE AT LEAST TWO PERSONS MUST BE INVOLVED
Many procedures need to be performed by at least two persons if asepsis is to be achieved: one (or more) performer within the sterile field, and another assistant / partner who works outside of the sterile field.
The practice of Aseptic Technique during some of the more common procures are discussed below.
Surgery – Minor and Major (operative team and circulating nurse)
Endoscopic therapeutic procedures (performer and assistant)
Endotracheal Intubation with an ET tube
The former performs direct laryngoscopy with a laryngoscope and identifies the glottis opening. The assistant should open the sterile pack of the ETT fully. The performer picks the external end of the tube and inserts the internal end directly into the trachea without touching structures in the mouth and throat (nor should he/she bend the tube on the bare OT table!). If for any reason the ETT tube need to be put down, place it back onto the sterile package looked after by the assistant.
Inserting a Central Line (performer and assistant).
The assistant introduces the IV cannula and all connecting tubes into the sterile field. Before the performer has inserted the cannula, he/she passes the end of the intravenous tubing (used to puncture the IV solution bag) to the assistant. The assistant connects the tubing to the bag and the fluid is run in to prime the line. The other end remains sterile in the sterile field and the performer then connects it to the intravenous cannula that has been inserted.
Inserting Chest Drains, Peritoneal Dialysis & Urinary Catheter
The assistant places all tubes and containers into the sterile field using a non-touch technique. The person inserting the tube should secure the connections before passing the containers (underwater seal bottles / urine containers / dialysate bags) to the assistant. Problems arise when the sterile catheter or tubes need to be connected to connectors outside of the sterile zone. In that situation the sterile (female) end is passed over to the assistant who will then connect it to the (male) connecter which has been kept sterile.
Performing Tracheo-Bronchial Suction on a Ventilated Patient
The aseptic technique is possible only if two care providers perform the task. One person disconnects and reconnects the ventilator tubing or Ambu bag to the endotracheal / tracheostomy tube. The other person performs the suction with a sterile catheter using both gloved hands.
When Delivering Babies
The risk of puerperal sepsis is always present (as was at the time of Semmelweis in 1847 Ref: http://en.wikipedia.org/wiki/Semmelweis). Normal spontaneous delivery may be performed by one obstetrician or midwife but for instrumental delivery (vacuum extraction or forceps) at least two persons is required. The instrument pack when opened should cover a whole trolley and more. The skin of the perineum and groin need to be cleaned with Cetrimide 3% or Chlrohexidine aqueous 1:200. Ref: http://en.wikipedia.org/wiki/Cetrimide. The obstetrician should wear a sterile gown. He/she need to drape the patient with sterile sheets exposing only the perineum and the introitus.
Managing the baby (resuscitation and so on) should be a separate procedure from the delivery itself.
Performing Wound Toilet & Dressing.
It is customary to name the two parties as clean nurse and dirty nurse. Perhaps it is better to call them inside nurse and outside nurse i.e. in and out with regards the sterile field.
The outside nurse opens the outer covering of the dressing set.
The inside nurse washes her hand and wears a pair of sterile gloves. She opens the inside layer of wrapper using her hands or the forceps provided.
The outside nurse now drops gauze pieces, cotton swabs, syringe and scissors into the sterile field created and after which she pours lotions into the galley pots. She then proceeds to remove the existing outer dressing on the wound.
The inside nurse should remove dressings within the wound with a pair of sterile forceps which she then passes outside. She then cleans the skin around the wound with 70% Alcohol or Chlorohexidine. The edge and base of the wound is cleaned with Chlorohexidine 1:200 solution. If MRSA is present Povidone iodine should be used and if it is Pseudomonas, it is customary to use Acetic acid. Sodium hypochlorite and hydrogen peroxide can be used for obviously infected wounds. The wound is flushed thoroughly with sterile saline or water using a syringe.
At the early stage of wound care gauze soaked in suitable antiseptic mentioned earlier or proprietary wound filler impregnated with antiseptic can be left inside the wound. Dry gauze or proprietary dressing is used for the external dressing and fixed with any type of plaster or a transparent dressing cover can be used.
When the wound is rid of infection then gauze moistened with saline or plain proprietary dressing is used. Otherwise, no gauze is placed in the wound but a roof of foam dressing or adhesive plastic is placed over the wound and left untouched for two or more days.
CONCLUSION
The practice of aseptic technique requires an understanding of the principles involved, adherence to proper procedures, use of the right resources and a proper environment. While vigilance and supervision is essential, compliance can only be achieved through individual commitment and attention to details.
I must point out my admiration for your kindness supporting individuals that must have help with this particular theme. Your very own dedication to passing the solution all-around came to be pretty functional and have constantly helped guys much like me to achieve their targets. Your own invaluable information implies a whole lot a person like me and even further to my peers. Thank you; from all of us.
LikeLike
Thanks, Doctor for this wonderful write-up.Please for reference purposes when did you publish this?
LikeLike
Thanks for the interest. I first wrote it on 4th August 2014. It has been updated, the latest being !9 June 2017.
Abdollah Salleh
On Sat, Jul 7, 2018 at 5:08 AM, Health Care Service Delivery wrote:
>
LikeLike
I first wrote it on 4th August 2014. It has been updated, the latest being 19 June 2017.
LikeLike
Thanks Dr for your support in facilitating better understanding of aseptic technique and the principles. I have a question. in an event that you as an inside nurse performing the dressing procedure and the outside nurse or the dirty nurse happened to pure aseptic solution on the sterile work surface, is the sterility of the aseptic procedure still maintained or not?
LikeLike
Antiseptic solutions are used to kill bacteria and are meant to be applied to wounds. They do not contaminate the sterile field.
When fresh, the solutions will not contain bacteria. However the remainder in the bottle/container may become contaminated after some time. If a solution is dispensed in a big container and reused many times, an in use culture and sensitivity test should be done. If there is bacterial growth, it should be discarded.
The better way would be to obtain from the pharmacy or buy from suppliers antiseptic solutions contained in small bottles/containers sufficient for use once or twice (within a day or two)..
LikeLike
Thank you for this article on aseptic technique Dr. Salleh. I believe these principles should be spread to and applied by the public especially with the current COVID-19 pandemic.
The only challenge there is on how to implement and inculcate these principles to our current and future people, as we all know this aseptic technique is usually only done by nurses and everybody in the medical field, not in normal situations by normal persons.
LikeLike
Thanks for your comments. We can start with the food industry. Food packaging industries and franchises are quite good but ordinary restaurants and hawkers don’t quite understand food hygiene. For Covid-19 the regular cleaning of surfaces frequently touched by people need closer attention.
LikeLike
Thanks for the wonderful write up. Bt I want to ask is aseptic also known as a sepsis???
LikeLiked by 1 person
Thanks for reading my article. Asepsis means ‘no sepsis’ or. a situation where pathogens (microorganisms) have not been introduced. I suppose aseptic technique is the way to establish the condition of asepsis.
LikeLike
This is good work…I truly understand more things through this work..I love it..may God increase you abundantly…..
LikeLiked by 1 person
Thank you
LikeLike
Thank you so much for valuable information
LikeLike