Date First Published: September 14, 2014
Date Last Revised: January 15, 2023
INTRODUCTION
In any industry a certain degree of uniformity and standardization of practice is required in order to maximize productivity, efficiency and quality. For most industries, this is achieved through documented plans called “Standard Operating Procedures (SOP)”. Patient care has developed its own approaches and terminology. The time has come to relate patient care practices to that of other industries in order to take advantage of innovations in the latter.
A study of current literature reveals the existence of diverse terms used in conjunction with the planning of patient care. The term Standard Operating Procedures is seldom used. In many instances, new terms are coined for the sake of being different to claim originality and therefore commercial value. A return to basic definitions of terms used in various areas of knowledge especially management science would lead to less confusion.
THE ROLE OF PLANNING IN OVERALL CLINICAL CARE PROCESSES
Planning is an integral part of the clinical work process. However. traditionally planning has been performed in an ad hoc rather than formalized manner. Currently, the need to regulate health services, streamline health care funding and ensure uniform quality of care, have resulted in wider acceptance of the use of standardized documented (ready-made) plans.
THE PLANNING METHOD
AD HOC PLANNING
Because of their training, healthcare professionals are capable of planning the care of a patient spontaneously. They rely on their knowledge and experience, and when necessary refer to practice guidelines, manuals and protocols or textbooks. Indeed, it is quite usual for clinicians, to think out a plan but not to document it. They express it only as orders or interventions.
There are many disadvantages of ad hoc planning (explained later). Yet, there are instances where preconceived plans are not available or inadequate and therefore the the skills of ad hoc planning need to be put to use.
The traditional way of writing a plan is as below:

In this example the findings and diagnosis is documented first. The plan is divided into two groups i.e. investigation plans and treatment plans.
SOAP Method
The plan is part of the popular Subjective, Objective, Assessment and Plan (SOAP) method of documentation. ‘Plan’ lies between the problem identification step (termed as ‘Assessment’) and actual intervention. The plan therefore is placed where it fits in the sequence of the clinical care processes. It is thought out only when the problem has been identified. An example is shown below:

Implementation and then re-evaluation follows the step of planning. The plan is changes as the case develops and rewritten.
The terms used is a bit confusing. ‘Subjective’ and ‘objective’ refers to the reliability of data based on the methods of obtaining them i.e. data from history taking is subjective while data from physical examination plus simple tests is considered to be objective. Many provider groups (nurses, therapists) use the term ‘assessment’ to refer to this step of gathering information and making sense of the situation. Medical practitioners use the term “formulating a diagnosis” for this step. In the context of the SOAP, assessment is best changed to diagnosis (‘deriving a conclusion’ or ‘formulation of diagnosis’).
Value of the SOAP Method
The SOAP method is a logical way of documenting the plan together with other clinical findings. As such, planning is not dissociated from other clinical care processes. However, this method is considered inadequate for the reasons that the reference for the plan is not available and therefore the plan is essentially ad hoc and not conforming to a standardized prescribed plan. This weakness can be overcome by providing care providers with prepared reference care plans (as will be discussed later).
Planning as Part of the Clinical Care Process
Traditionally, planning is part of the series of processes in the delivery of patient care occurring only after the diagnosis is made (described in another article).

It would appear that planning is an ad hoc process. It is made by the clinician based on his/her knowledge and experience. The use of more structured formalized plans is necessary.
STRUCTURED FORMALIZED PLANS
Current Attempts at Creating Care Plans/Care Pathways
For many years now some sectors of the healthcare service notably nursing has advocated more formalized prescribed methods termed as Care Plans or Care Pathways. Some models are very detailed and incorporate nearly all care processes. Others are just outlines with minimal content leaving it to the care provider to expand the plan. Many of the approaches and methods are still valid and should be retained as the basis for further development.
An appraisal of the two basic models in current use is given below.
Model A
In this fairly popular model, the plan takes the form of a table. The contents include:
- Results of assessment of available information
- Problem identification ( diagnosis and effects)
- The rationale for the plan
- Proposed interventions
- The expected outcome
- Method of evaluation of actual outcome
An example such a Care Plan is given below:
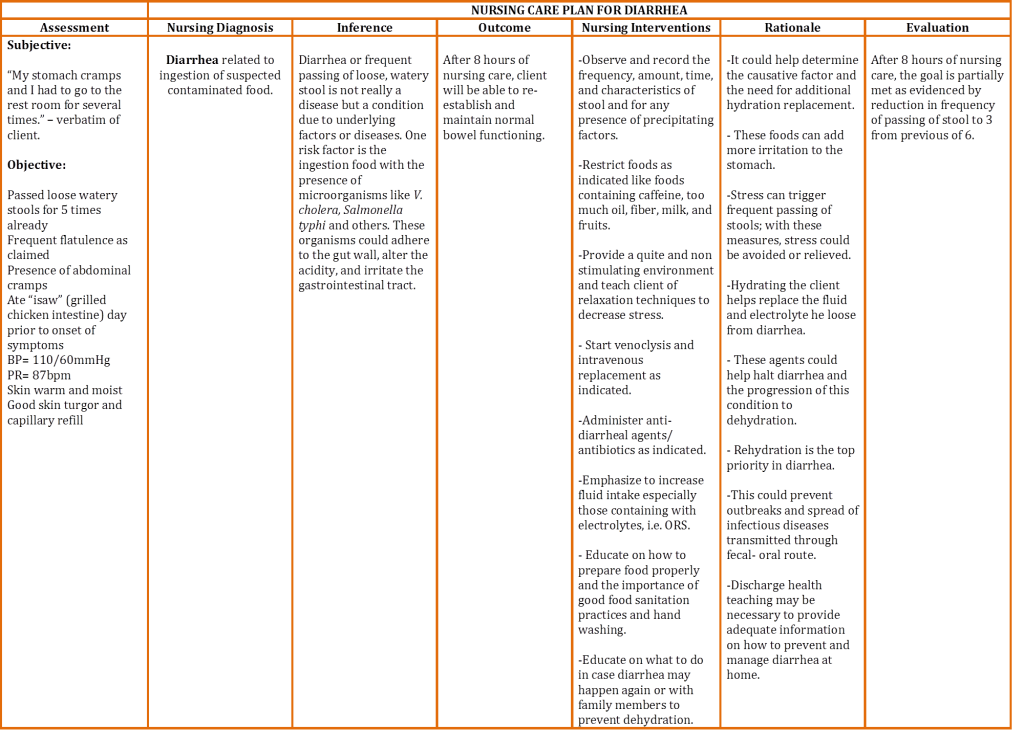
The plan is made in ad hoc manner based on the findings and diagnosis made. The documentation of the results of assessment, interventions and the actual outcome is deemed to be part of the plan
The format of this model makes it useful as a reference and for educational purposes. However, it is not suitable for practical use. The plan and actual processes should be documented separately. Often however, there is an attempt to document the actual care given in a similar (table) format. This is improper because the notes will not be in chronological order. The task of planning and the documentation should not be mixed with other care processes. Notes should be written as and when tasks are performed. To overcome this shortcoming, some hospitals advocate that notes are written both in the SOAP format and the table format. This results in redundant work for nurses.
Model B
More commonly used is a less complicated model where the nursing diagnosis and the corresponding planned interventions (tasks to be performed) are indicated as instructions. However, there is still a failure to differentiate the plan (instructions) from the task execution and actual findings of observations, monitoring and evaluation. They are often written together with the plan in table format.
Again to overcome this shortcoming, notes are written both in the SOAP format and the table format. This leads to duplication of documentation efforts and confusion.

Lessons Learned from Currently Advocated Plans
The plan in Model A is meant to be a reference. This is obvious from the inclusion of rationale, inference, interventions to be performed and what to evaluate in the content.
Model B exemplifies an attempt to document diagnosis, task performance plus their results/findings according to the format of a plan. As such it is a record not a plan. It is done in this way because care providers (especially their supervisors) want to see the plan and the corresponding record displayed at one place within the medical or nursing record. This requirement is also the reason why the plan is structured as a table or matrix. However, the choice of this layout leads to unwieldy Care Plans that are cumbersome and confusing to use because of the limitation in the amount of information that can be included in the many narrow columns. Again, despite the use of a matrix, it is also often mistakenly called Care Pathways which are actually algorithms..
The Need to Document Planning and Their Execution Separately
Planning and carrying out interventions are separate clinical care processes performed in chronological order. Therefore, the plan should be documented first. The tasks performed and the findings are recorded later when they are done or when the results are evident. Indeed they should be recorded in the medical record in a chronological order (as per legal requirement). If the wish is to present the plan and the actual interventions at the same place, then care providers have to transcribe (duplicate) what they have written as notes in the medical record into a separate table as a summary. This duplication of effort is the main grouse cited against current care plans.
USE OF STANDARDIZED CARE PLANS
Until recently these care delivery plans are often developed by certain categories of healthcare providers notably nurses. There is now an increasing awareness for the plans to be interdisciplinary. Advocates in the United States emphasize this change in approach by calling the plans Interdisciplinary Client Plans, Critical Pathways, Interdisciplinary Outcome Pathways and many other terms. Somehow, there is a general lack of understanding regarding the meaning of the terms ‘Care Plans’ and ‘Care Pathways’ and the context within which they are to be applied in the delivery of health care. Indeed there is a lot of controversy, confusion and inconsistency regarding the use of care plans and clinical documentation within the nursing profession.
Understanding the Terms used in Planning Healthcare
Clinicians use the term ‘management of a patient or case’ to refer to the provision of the clinical service of a patient affected by an illness. The term ‘care’ is more appropriate for the clinical aspects of the service. Some of the terms used in planning is as below:
Case Management: Patient administration or patient management is widely used to refer to the administrative aspects of care. On the other hand, the term Case Management is used by certain health care practitioners to mean the entire care across episodes and inclusive of services not necessarily clinical in nature.
Plans: The general meaning is the arrangement in advance on how to carry out a certain activity. There are slight variations when applied to different endeavors. In architecture, it refers to a representation of the intended physical structure and layout. In management, planning is defined as the activity of selecting strategies, methods, policies, programs to achieve defined objectives. Planning refers to either one or both sequential activities i.e. Structural Plan (Design) and the Implementation Plan (Schedule, Process layout).
Algorithms: When used in mathematics, it is the step-by-step procedure for solving a mathematical problem in a limited number of steps. When used in other areas such as patient care, it is the series of sequential decision-making thought processes in managing a clinical problem based on some rationale. The sequence can be iterative (cyclical) where previous processes are repeated.
Pathways: Clinical pathway is another term for algorithms when it is used in patient-care activities. It is the predicted or planned series of logical steps in managing a clinical problem, from the beginning to the end. As work progresses, a decision making step determines the subsequent alternative series of steps. Part of it deals with process layout e.g. whether simultaneous or sequential. Indeed, Care Pathways are depicted schematically as flow diagrams or charts together with a narrative. A Critical Pathway contains only the critical (important, required) steps or processes with the obvious (mundane) steps left out in the documentation (but not in practice). It is incorrect therefore, to call a pathway a plan. In practice the pathway is didactic but often contains alternatives chosen by the care provider.
Work Flow: Work Flow is depicted schematically as charts made up of flow diagrams written together with a narrative. It should be differentiated from algorithms and pathways. The latter being a thought process can proceed is a recursive way (i.e. the same thought process is repeated). Whereas, processes in workflows should progress in a forward direction as new actions. It may be a repetition of previous processes but at a different period, within a different circumstance and possibly by a different person.
Work Schedule: Schedules are sets of care packages usually depicted as lists containing tasks arranged, bundled together and sequenced according to the workflow. The schedule provides direction to the clinical team on tasks to be performed according to scenarios, occasions, phases of care and events guided by professional, quality and safety requirements. Even though traditionally, schedules are equated with plans. a plan is more than just a matrix or table.
Practice Guidelines: These are written documents prepared by experts outlining broad recommendations for management of patients with a disease condition based on scientific evidence (research) available in the literature. They vary in detail and specificity, depending on the complexity of the disease and degree of variation in its presentation and in treatment possibilities. (Refer: Cochrane Collaboration)
Reference:
Meaning of pathway
ADVANTAGES OF USING MORE FORMALIZED PLANS
Objections to Use of Standardized Plans
In the past and to some extent even today, many health care providers question the need for uniformity and standardization for the following reasons:
- Each patient is very different from another and therefore the care of every patient is special (they claim that design should be on a patient to patient basis; standardization leads to “cook-book” medicine which is considered as dangerous)
- Clinicians need to make independent decisions in choosing management strategies and actions (according to them plans curtail clinical freedom)
Generally, despite these concerns, there is wider acceptance of the need for standardized plans among healthcare providers. In fact, over the years, they have developed many tools for planning patient care and many have been widely used. However, the structure and content of such plans have not been uniform.
Learning from Other Industries
To help improve the understanding of the planning process, it is proposed here that effective and well-accepted modern approaches and techniques in operations and quality management as used in other industries be adopted in health care.
Much need to be learned from other industries. It is imperative that strategies, methods and mechanisms that have been proven effective in various industries be adopted, after careful consideration of their applicability. In manufacturing industries, operations management is concerned with the production of a specific product. The concept of a service product and clients/customers, already entrenched in banking, insurance, hospitality, tourism and sales, needs to be embraced by health care providers because it allows for the quality of a service to be defined by characteristics that are measurable and can be replicated . Indeed, there are more similarities than differences in the approach and in the terminology used. A comparison of the terms used is given below:

Care Plans
There is a need to move away from the design and implementation of care plans as commonly practiced. Care plans should be taken as the equivalent of the Standard Operating Procedure (SOP) used in other industries and be used in the same way, The difference is that while industrial products ave rigid specifications and their method of production is always consistent. Health care outcome and their delivery are subjected to many variations which can be quite complex. The way to overcome this difficulty will be discussed.
Advantages of Standardization
For the care provider, the use of formally designed (prepared) SOP/Care Plans provides many advantages including:
- Facilitate a more structured care delivery
- Ensure comprehensive (complete) content of the service
- Encourage appropriate selection of investigations and treatment; remove redundancy or duplication and wastage
- Provide information and decision support (through suggestions, prompts and reminders)
- Give a clear picture of future actions
- Communicates intentions to the whole care team (thus encouraging shared objectives and understanding)
Standardization promotes uniformity in the care of patients suffering from similar disease, syndrome or symptom complex, among all care providers and at all facilities within the same organization. The reference SOP/Care Plan is a guide. Allowance for variations is written into the plans. Even so, it does not in any way discourage practitioners from altering practices in response to peculiar situations and requirements.
Towards the Development of Formalized Plans
Just as in manufacturing industries, businesses providing services called what they deliver to customers as service products. This approach makes the the characteristics of the service more uniform and distinguishable.
Varied Nature of Clinical Patient Care as Service Products
In other industries the product of manufacturing or service delivery are very well defined and so also are the input and processes used. This is not so in healthcare. While care can be made uniform based on the patient’s disease, the needs of patient varies quite significantly depending on many factors. It would seem that there as many service products as there are diseases. These would have to be further broken further into more specific service products based on:
- Diagnosis
- Care Objectives
- Different Phases of the Clinical Care Process.
Diagnosis would be the main determinant of the service to be delivered to the patient. During the course of patient care, the amount and clarity of information available to the care provider increases and the diagnosis becomes clearer or new problems emerge. Diagnosis can take the form of:
- symptom complexes,
- clinical syndromes.
- diagnostic related groups,
- specific disease, illness or health problem and
- variants of the disease.
Plans need to be developed for all of them.
This complexity in types of service products can be resolved by building a generic plans that contain the required parts and from there adjusted to suit the requirements posed by grade, severity, stage, presence of complications and other additional requirements. The approach must be to design standardized plans that are generic in nature i.e. applicable to typical patients with a typical disease condition. They are used initially as a reference and are then customized before being applied to the actual care of an individual patient. If the patient has more than one health problem, then combination of the generic plans would be necessary.
The subject of Planning of Clinical Patient Care will be discussed further in three more articles
- The Development of SOPs and Care Plans
- Documentation of SOP/Care Plans
- Implementing SOP/Care Plans