Date First Published: July 22, 2014
Date Last Revised: July 4, 2023
INTRODUCTION
The Total Patient Care concept and approach refers to the provision of services catering for all the needs of the patient including physical, psychological, social and spiritual needs. It means managing the patient as a whole. Sometimes this approach is referred to as the practice of “holistic medicine”. To put the concept into practice requires clear objectives, strategies and approaches. The concept may be applied for two obvious purposes i.e.:
- as a description of all the features and components of patient care
- as a framework for a comprehensive and integrated patient management plan
COMPONENTS OR ELEMENTS OF PATIENT CARE
The provision of care involves the primary act of caring as well as other services that facilitate this activity.
Patient care activities can be categorized into:
- Clinical Patient Care
- Hospitality Service
- Administration and Communications
The discussion below centers mainly on clinical patient care and attempts to demonstrate the importance of the other components of patient care.
CLINICAL PATIENT CARE PROCESSES
Clinical Patient Care coonsists of a range of processes that include:
- Generation, gathering and collection of data about the patient and his/her disease
- Analysis and interpretation of data to determine the diagnosis and needs of the patient
- Planning the case management
- Treatment
- Review of the progress of the disease
- Monitoring of the effects of treatment
- Review of diagnosis and management
- Continuation of care or final disposal of the case
Each of these processes are described briefly in this artic;e and will be discussed in further detail in separate artticles at this site.
CLINICAL PATIENT CARE WORKFLOW
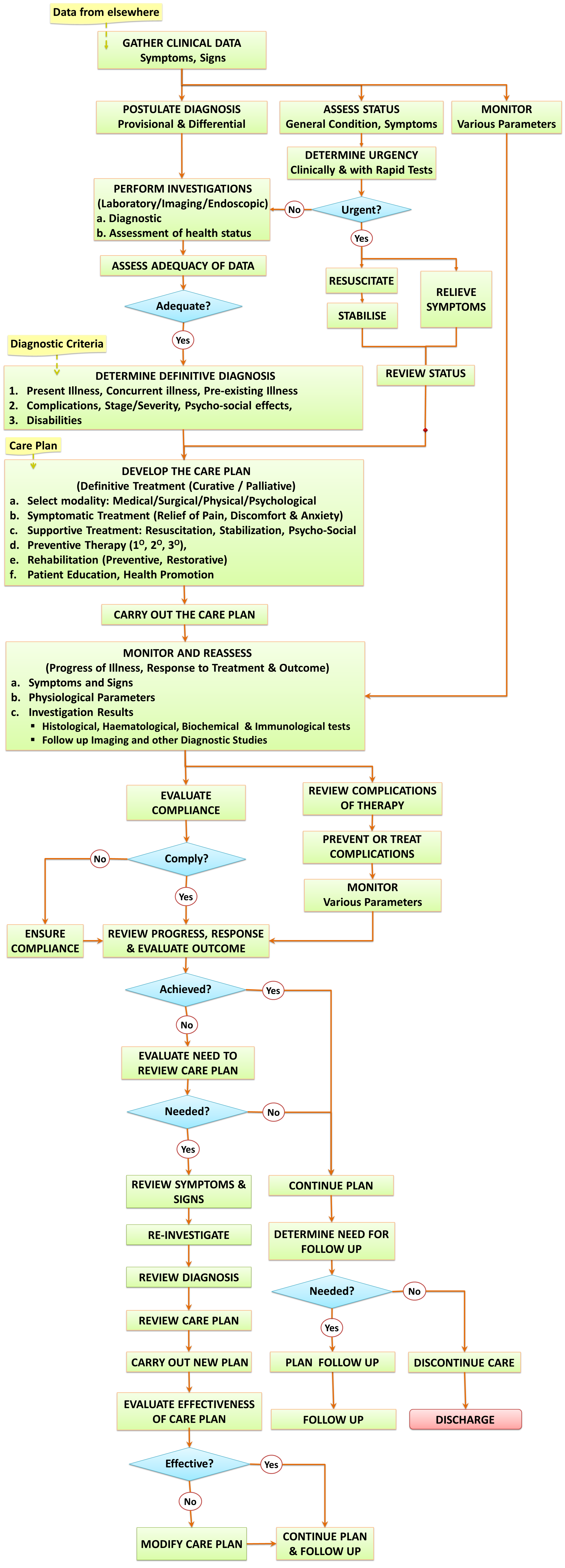
An outline of the sequence and relationship of these Clinical Patient Care Processes is shown in the Algorithm below. This algorithm can be modified to draw up a workflow or Critical pathway of Management for various types of cases.
Clinical Care Workflow
DATA MANAGEMENT IN PATIENT CARE
CLINICAL PATIENT CARE AS DATA MANAGEMENT ACTIVITY
Clinical Patient Care can be considered as a management exercise. Typically, a care provider gathers data by various means. He or she then interprets the data by comparing them with his or her knowledge. This enables him or her to derive conclusions, the most important of which is the diagnosis. Based on the diagnosis, the case management plan is selected or constructed. Action is taken based on the decisions. Gathering of data is continued to monitor progress and to provide feedback on the outcome of the care given.
Results of analysis and interpretation plus the conclusions derived are also recorded as data.
| Data Process Steps | Clinical Care Process | Data |
|---|---|---|
| Data gathering | a. Interview (history taking) b. Physical Examination c. Tests and Investigations d. Monitoring e. Progress review | Symptoms Signs Test results Parameters Progress |
| Data Analysis & Interpretation | a. Formulate the diagnosis b. Formulate plans | Diagnosis Care Plan |
| Deriving conclusions | a. Declare the Diagnosis b. Progress c. Outcome of care | Diagnosis Progress Outcome |
| Making decisions | a. Choice of methods | Care plan |
WAYS OF GATHERING DATA AND SOURCES OF DATA
Caregivers normally generate data by performing the tasks listed below and recording them either as notes, results or charts.
- Interviewing the patient (taking a history)
- Physical examination
- Simple clinical tests
- Investigations including laboratory, imaging, endoscopy and others
- Monitoring and
- Assessment
It is also important to retrieve and review existing data from the medical record and data from other sources e.g. referral letters from the previous care provider.
Data management is discussed further in another article
Amount and Type of Data To Be Collected
In the context of total patient care, data must be:
- sufficient,
- appropriate,
- accurate, and
- provided in a timely manner.
Care givers must collect sufficient data for the purposes of:
- building the patient profile
- establishing the scope of care
BUILDING THE PATIENT PROFILE
A patient profile is a complete set of data regarding the patient which will. form the background information essential for managing him or her. Every attempt must be made to gather as much relevant information as possible to enable proper analysis, interpretation and decision making. These include:
The amount and type of data required and the content of the subsequent management plan are determined by:
- demographic data
- current (premorbid) health status
- lifestyle and activity level
- education level
- knowledge and attitude towards health
- social situation
SCOPE OF CARE
The scope of Clinical Patient Care covers all aspects of the patient’s health i.e.
- Present illness
- complications of present illness
- physiological effects of the illness
- psychosocial effects of illness
- Concurrent illness
- Preexisting illness
- Unresolved past illness
Besides data on the nature of the illness, the patient profile mentioned earlier is important.
It may not be possible or necessary to gather all this information all at once at the beginning of the patient’s visit, The profile of the patient and his/her needs should be built initially and updated as more data is accumulated during the provision of care.
Clinicians put together and analyze all these data, interpret them, derive conclusions and make decisions.
Throughout the care of the patient more data are collected to monitor the success of treatment and progress of the illness.
DEVELOPING A COMPREHENSIVE CARE PLAN
The design of an integrated care plan, catering for all the needs of the patient, must be based on the analysis of adequate information. The immediate result of analysis is a conclusion regarding the nature of the illness, which in clinical patient care is termed as the diagnosis. The accuracy of this diagnosis is of course very dependent on the completeness and quality of available data. Clinicians describe the degree of accuracy qualifiers such as:
- provisional,
- working,
- presumptive, and
- definitive.
The development and use of Care plans is discussed further in another article
DIAGNOSIS: THE KEY TO COMPREHENSIVE CARE
Traditionally the term diagnosis is often restricted to the disease that afflicts the patient currently. However, if complete care is to be given, the diagnoses should also describe the way his/her current illness has affected his physiology and psychology, the existence of concurrent illness, preexisting disease and unresolved past problems that have bearing on the current problem. This more comprehensive diagnoses provides a clearer perspective on how subsequent care processes are planned.
Therefore, the components of a comprehensive diagnosis would include:
- Present/Current illness
- Primary Present illness
- Concurrent Present illness
- Preexisting illness
- Chronic illness
- Unresolved previous illness
- Preexisting health status
- Nutritional status
- Psycho-social status
- Past Illness
- Past disease
- Past trauma
- Past surgery / procedure / anaesthesia
- Disabilities and Handicaps
The current illness is the usual reason for seeking health care but may not necessarily be given the highest priority. Sometimes problems related to the concurrent illness or complications of the preexisting illness is more pressing.
SEVERITY OF ILLNESS AND STAGING
In the assessment of the present illness it is important to determine the severity of the illness, based on the stage of the pathological process (extent and duration) and the degree of:
- alteration of the patient’s physiology,
- distress caused by symptoms,
- disability as the result of illness,
- nutritional deficit,
- psychological upset
- social disruption
The severity and stage of the illness are also important factors in deciding on the choice of the most appropriate treatment approach and modality.
The topic of Diagnosis is discussed in detail in another article.
OBJECTIVES AND CONTENT OF CARE
CARE OBJECTIVES
It is important to determine the care objectives at the start of patient management and review them at subsequent phases. While definitive treatment preferably should be started only when an accurate diagnosis is made, much can be offered to the patient in the meantime.
A wide variety of strategies, methods and modalities are available to the care provider. Their selection depends on the treatment objectives and may include any or all of the following:
- Remove or minimize effects of illness
- Maintain, restore or improve the health status
- Avoid or minimize complications of treatment
- Prevent deterioration or recurrence
Depending on the nature of the disease and the objectives, the treatment strategy can be one of three categories:
- Curative
- Restriction of effects and prevention of deterioration
- Palliative
When there is potential for cure or cessation of the disease processes, a concerted attempt is made to achieve it. However, even when there is no possibility for complete resolution of the illness many different therapeutic interventions can be offered.
Each of the three categories has several common components or content i.e.:
- Symptomatic therapy
- Supportive therapy
- Preventive therapy
- Rehabilitative therapy
- Health Promotion
The priority and sequence of treatment will depend very much on the type, severity and effects of the illness.
| “…to cure sometimes, to relief often, to comfort always ”Ambroise Pare’ (French surgeon 1510-1590) |
PHASES OF CARE
The period within which care is given to a patient with a particular health problem or disease is termed as the care episode. This can be divided further into sequential phases of care which vary according to the stages of the natural history of the disease (or disease episode) such as:
- The disease onset and progression:
- whether acute, sub-acute or chronic
- The optimal target (end-point) that can be achieved:
- cure
- arrest of progression (modify, moderate, ameliorate)
- prevention of further complications
- recovery of lost function
- palliation
Each phase has its own objectives and content depending on the needs of the patient. The care in each phase may comprise one or more care visits and encounters with the relevant care providers in the appropriate care setting (in-patient, daycare, out-patient, or home visit services).
Schematic representation of examples of Phases of Care are shown below:
Phases in the Care Episode of a Chronic Illness
Phases in the Care Episode of an Acute Illness
MANAGING SYMPTOMS
Symptoms such as pain, thirst, hunger, discomfort, physical disability including impaired movement, inability to perform activities of daily living, anorexia, vomiting, diarrhoea, constipation, insomnia, anxiety, depression, feeling of insecurity and inability to communicate well are foremost on any patient’s mind. These require prompt attention by caregivers while efforts aimed at determining the definitive diagnosis are in progress. It is important to monitor and review these symptoms. The timely relief of these symptoms may not necessarily be drug treatment but simple nursing care may suffice. Management of these problems are provided through nursing care, physiotherapy occupational therapy and efforts at improving social adaptation.
Managing Disability and Dependence
The degree of a patient’s disability should be assessed. The likely disabilities include:
- assessment of the ability to perform activities of daily living (ADL) which can be documented as a ADL score.
- disturbances to the senses pf smell, taste, touch, sight and hearing
- limitation of movement and physical strength
- disability of speech
- disorder of thought processes
- psychological disturbance
Results of the assessment will help determine the patient’s level of dependence on care providers. It also indicate the type of rehabilitative efforts to be undertaken.
RESUSCITATION AND STABILIZATION
Patients suffering from serious acute illness and those with acute complications of their chronic illness may have deranged physiology. These can be life-threatening. Detection and correction must be swift. Resuscitation includes correcting hypovolaemia, electrolyte imbalance and improving functions of the various systems especially the respiratory system, the circulation, haemostasis, renal and neurological function. Efforts must be made to improve and sustain (stabilize) the physiological status at an acceptable level.
OPTIMIZATION OF NUTRITIONAL STATUS
The nutritional status prior to illness, the effect of the illness on appetite and the ability to eat and drink should be assessed. It is also important to ensure that the patient receives adequate and balanced nutrition as part of his/her management. Nutritional support is especially crucial if the disease affects the gastrointestinal tract and when the treatment involves surgery, chemotherapy or radiotherapy.
PSYCHOLOGICAL ASSESSMENT & THERAPY
The patient’s psychological well-being is as important as the physical aspects. His/her premorbid mental state and the effect of the illness on it needs to be assessed. The care provider needs to be sensitive to the patient’s ability to cope with the current illness and treatment. Patients have varying levels of dependency on care givers to perform normal tasks including simple activities of daily living. Anxiety and depression often accompany an illness. Patients often refrain from voicing out their needs out of shyness or reluctance to burden care providers of ‘extra work’. Being dependent on others brings about distress to the patient. Some, therefore, suffer in silence. Care givers need to be sensitive and responsive to these needs. Aid should then be provided promptly and consistently. Explaining the nature of illness and reassurance is essential. The way the disease affects the social life of the patient requires due consideration. His/her illness will affect his ability to communicate, relationship with family, friends and other people he normally interact with. His/her ability to perform work or other activities is often impaired.
The psychological state of the patient must be continuously assessed during care. The illness and the processes that the patient have to go through can be overwhelming. Care providers must look out for the emergence of anxiety, depression and suicidal tendency.
CURRENT HEALTH STATUS & OTHER ILLNESSES
The patient’s concurrent and preexisting illness should be given as much attention as his or her primary current illness. Patients presenting with an illness involving one system may well be suffering from pathology in other systems. For example a patient with Acute Cholecystitis or Perforated Appendicitis may also have Pneumonia which if undetected may result in poor outcome. A pre-existing illness could be identified at the time of clerking if the patient is already aware of them. Attempts should be made to obtain past records so that ongoing treatment can be continued. In certain situations, treatment may have to be discontinued temporarily or altered.
SCREENING FOR COMMON CHRONIC ILLNESSES
When there is no previous history, common chronic illnesses should be screened for as part of patient assessment through clinical and investigative means. When detected, treatment should be initiated (after consultation if necessary) and continued beyond the period of care of the present illness. Common chronic illnesses include:
- Bronchial Asthma / Obstructive Airway Disease
- Diabetes mellitus
- Hypertension
- Ischaemic Heart Disease
- Renal Impairment
- Chronic skin problems
- Psychiatric illness
NEGLECTED AILMENTS OR HEALTH DEFICIT
Quite often patients suffer from various ailments or health deficit for which they do not seek treatment or advice either because they consider them trivial or did not realize that medical help is necessary or is available. Common neglected ailments or health deficit include:
- lack of or incomplete immunization for children,
- poor dental care
- skin problems
- worm or other parasitic infestation
- nutritional problems (anaemia, obesity)
- psychiatric disorders
- disabilities, impairments, handicaps and deformities (limbs, vision, hearing, speech)
ADVOCACY
The caregiver needs to act as an advocate and attempt to educate patients and to alert them regarding the need to seek attention to the health problems identified. When requested by the patient and with his/her consent, the caregiver should provide the help required or direct patient to the appropriate sources of care by formally referring the patient or otherwise. At the beginning of care patients should be told of their rights and they should be given opportunities to air their grievances. Often patients encounter difficulties and hindrances with policies, procedures and amenities of the the facility. These need to should be looked into sympathetically.
PREVENTION AND SAFETY
Prevention of complications and ensuring safety are fundamental aspects of clinical case management. A patient already suffering from an illness is exposed to the possibility of contracting other illnesses or injuries. Modern medicine has many benefits but also has the potential of inflicting harm. Each mode of therapy has their pre-requisite requirements, safety features and side-effects.
Primary prevention refers to the prevention of a possible illness or injury from happening. Eminently preventable common illnesses include Pulmonary atelectasis and Deep Vein Thrombosis, muscle wasting and joint stiffness, to name a few. Anticipation of the possibility of untoward effects, for example allergic reactions or suicidal tendency), can help avoid their occurrence. In a hospitalized patient, serious efforts must be made to prevent conditions such as pressure sores, eye injury, and nosocomial infections. With due care complications of therapy such as medication error and surgical complications can be averted.
Secondary prevention refers to the limitation of harm caused by the illness. These include measures to stop the disease from progressing to a higher level of severity, limiting the duration and degree of suffering and preventing disability. Unavoidable or unexpected complications require prompt and appropriate response. Tertiary prevention refers to restoration of lost function and the arrest of further deterioration of disability.
REHABILITATION
Rehabilitation is an important component of patient care and begins at the very onset of care. It has both a preventive as well as corrective function. The patient’s type and degree of disability must be assessed. The appropriate rehabilitative efforts are started and continued until various functions are optimally restored or disability maximally reduced..
The objective of rehabilitation is to return patient to society as a useful member with a good quality of life.
Rehabilitation involves:
- physical rehabilitation
- improving cognitive function
- psychological support, counseling and therapy
- social adjustment and socioeconomic aid
The responsibility of carrying out the above measures does not lie only with Physiotherapists, Occupational therapists or Counselors. It should be considered a part of the day-to-day duties of doctors, nurses, and other allied-medical staff.
PATIENT EDUCATION
Patient education should be included in the management strategy of every patient. Education is aimed towards ensuring that the patient understands:
- the nature of his/her disease or illness,
- the methods used by the caregiver to alleviate the illness
- the patient’s role in the management of his/her health
The activity of patient education is part and parcel of the services provided by every category of care provider. It can be given informally or through organized sessions.
Orientation and giving information (regarding admission procedures, visiting hours, payment etc.) must be differentiated from education. These are basically administrative procedures and communications.
INVOLVEMENT OF PATIENT, FAMILY & OTHER CARERS
The involvement of patients in the process of care is made possible if they are given adequate information and encouraged to participate in the care of their own illness. Well-informed and motivated patients are more likely to comply with treatment, be able to practice self-care and would be less likely to misinterpret undesirable outcome. Where relevant, education and training is also given to the patient’s family or other carers.
HEALTH PROMOTION
A patient’s visit or admission to the hospital or health facility should be seen as an opportunity for health promotion. This can take the form of imparting knowledge and advice on all aspects of health not necessarily related to the present illness. These aspects include:
- practice of a healthy lifestyle
- hygiene
- nutrition
- disease prevention i.e. immunization, accident prevention, family planning, and healthy lifestyle etc.
MONITORING, EVALUATION & CONTINUITY OF CARE
MONITORING
Monitoring is an important component of the clinical care processes. It provides information on the progress of the illness.It links the problem identification phase with the treatment phase by providing feedback and thus dictating the direction of subsequent care. The aspects that require continuous monitoring includes:
- The patient’s health status,
- Progress of the illness including effect of treatment on the illness,
- Unwanted or side effects of therapy.
To achieve this goal, monitoring need to be performed consistently from the start and end only if the disease is considered cured or the care has been discontinued.
Monitoring is directed at assessing certain relevant parameters and for each parameter, an appropriate method of measurement is used. These include:
- Regular review or observation of symptoms and signs
- Repeated measurement and charting of physiological parameters
- Serial measurement of biochemical parameters
- Repeated of Microbiological and Haematological tests
- Follow-up Imaging studies
- Reassessment using diagnostic studies such as endoscopy etc.
Monitoring intervals are matched with the character of the illness. For some illness, regular observations of symptoms and signs provide the best guide as to whether the patient’s health is improving and may also be a reflection whether the disease process is on the decline or is actively progressing. Acute illness with tendency for rapid deterioration requires continuous monitoring techniques or constant observation by alert care providers.
Measurements of each parameter recorded in the form of a table or chart shows progression and trends. Sudden changes may require urgent intervention. Subtle changes require careful study before decisions to intervene are made.
Monitoring is discussed further in another article.
PROGRESS REVIEW
Evaluation or re-assessment of the patient’s status and also the progress of various treatment programmes need to be done continually. It is performed as part of the procedure of “Progress review”. It is meant to provide answers to the following questions:
- Have all the needs of the patient been attended to?
- Have all the planned actions been carried out?
- Have the objectives been met?
- What more need to be done?
The scope of evaluation of care includes:
- review of progress of disease,
- monitoring of effects of treatment,
- review of diagnosis,
- review of treatment,
- evaluation of outcome.
Various methods used in the initial assessment of illness i.e. clinical data gathering and various investigation modalities can be performed repeatedly in re-evaluation. To obtain an accurate appraisal of progress, the care provider needs to put together data from various parameters being monitored and carefully analyze them. Some diseases require close monitoring using specific special tests e.g. tumour markers.
Monitoring of Various Diseases
However, for some diseases deterioration or recurrence is less clear but hinted by non-specific symptoms, signs or biochemical changes which are discernible only to the alert clinician with a high index of suspicion.
EVALUATION AND DETERMINATION OF OUTCOME
While monitoring and assessment is performed on a continuous and regular basis, there is a need to determine and document the outcome of care using universally accepted indicators or scores suitable for the disease or health problem. The documentation must be done at certain milestones corresponding to the phases of care. This could be at the end of inpatient care (to be documented in the discharge summary), at a predetermined follow-up outpatient visit or at the end of a care episode. Although the final outcome is important, it is as important to document the intermediate outcome because it provides an indication whether the desired objectives are being met and therefore allow for changes to be made to the care plan if required.
The documentation of outcome provides the data for quality assessment of the service given to an individual patient as well as for a population of similar patients through medical audit.
CONTINUITY OF CARE
An important feature of holistic care is the continuity of care. Continuity ensures that management of the patient proceeds according to plan. It prevents initial gains of various treatments from being lost and provides opportunities for re-evaluation. Clinical care processes that ensure continuity include:
- adequate and timely follow up,
- planned after-care,
- expectant management (early detection of recurrence or of long term complication).
As care is provided usually by many providers, it is essential for good communication to be maintained through:
- accurate and complete documentation in the patient record,
- effective handover,
- well written referral letters,
- sharing of case summaries,
- easily understood oral or written instructions to patient or care providers.
It is also important that a clinician (doctor or nurse) is designated as the primary or main care provider and given the responsibility for coordinating care. Care providers must ensure that when a handover is necessary, (e.g. at the start of shifts or takeover of care by a different person) adequate information is exchanged. Besides sequential continuity, another important aspect is ensuring that treatment provided by diverse care-providers follow a common objective and plan without duplication or conflict.
DOCUMENTATION
It is a medico-legal and professional requirement for care providers to maintain a chronological record of all clinical activities and all events that happen during the period of care (compiled as the Medical Record). Each care provider must ensure that the documentation is accurate, complete, and easily understood.
Documentation is also necessary to enable the following:
- allows for the sharing of information among care providers,
- facilitates continuity of care
- make available data for clinical audit, quality assurance, managerial decision support, epidemiology and research.
ADMINISTRATIVE PROCEDURES AND COMMUNICATION
Administrative procedures and communications also must be carried out efficiently and effectively to ensure patient satisfaction. These procedures include:
- Registration and Admission procedures,
- Briefing and Orientation,
- Taking Consent,
- Billing,
- Discharge procedures,
- Scheduling.
All these procedures should be tailored to meet the needs of the patient. Communication is of critical importance. Misinterpretation may cause in non-compliance, errors or delays resulting in less than desirable outcome.
Front line staff carrying out administrative duties e.g. receptionists, clerks, security personnel must be sensitive to the needs of people with health problems and have an understanding of the clinical process of care. Clinical staff on the other hand must also be familiar with administrative procedures and be ready and willing to render assistance.
HOSPITALITY SERVICES
Hospitality services must be provided adequately and in such a way as to give patient and their relatives/friends maximal comfort and with respect for personal dignity, privacy and confidentiality. These services include:
- Reception,
- Lodging,
- Food and beverages,
- Comforts,
- Privacy, Safety and Security,
- Entertainment,
- Information,
- Communications utilities,
- Transport facilities,
- Facilities for social interaction,
IMPLEMENTING THE TOTAL PATIENT CARE CONCEPT
Adoption and implementation of Total patient care requires applying the concept in all aspects of health care delivery.
Optimal benefits of health care can be achieved through teamwork. Policies and procedures that enable and value the contributions from all health care professionals, the patient and relatives need to be created.
This concept can be translated into practice using the following strategy:
- use a combination of approaches,
- involvement of a team of care providers,
- enabling integration,
- facilitating co-ordination,
- providing for continuous assessment.
TEAM MANAGEMENT OF PATIENTS
The best way of implementing this concept is the use of a comprehensive Care Plan (Case Management Plan, Standard Operationg Procedures). The plan addresses all aspects of the patient’s health problems in the short-term as well as the long-term. Conceptually, the care plan is a matrix where various patient care activities are plotted against time. The people involved or responsible for the various activities are also indicated. This care plan can remain conceptual in the minds of the provider or it can be written down in the form of a table.
Patients are categorized based on the diagnosis and its severity. Individualized care plans are derived from generic plans. The designs of these generic care plans requires contributions from all health care professionals involved in the care of each patient category. This can be achieved through the formation of Interdepartmental or Cross-Functional teams. Current Clinical Practice Guidelines can be the basis for these generic plans but very few of these have been developed according to the Total Patient Care Concept. The framework for a generic care plan based on the total patient care philosophy is shown below.
Framework for Patient Care Plan

The topic of Care Plans is discussed in another article.
and further in



Leave a Comment