Importance of Monitoring Intake and Output
Monitoring is an important clinical care process that provides the means to determine the progress of the disease and the beneficial as well as detrimental effects of treatment. Monitoring of intake help care givers ensure that the patient has proper intake of fluid and other nutrients. Monitoring of output helps determine whether there is adequate output of urine as well as normal defecation.
Purpose of the Intake-Output Chart
The intake and output chart is a tool used for the purpose of documenting and sharing information regarding the following:
- Whatever is taken by the patient especially fluids either via the gastrointestinal tract (entrally) or through the intravenous route (parenterally)
- Whatever is excreted or removed from the patient
Sometimes it is known as the Fluid-Balance Chart.
Because the amount is measured in standard measuring units (usually in ml), some calculation such as addition, subtraction and totaling can be done.
The Physiologic Basis for the Intake-Output Chart
Indirectly, the chart gives an idea of the status of the patient’s physiology including:
- Gastro-intestinal function (ability to eat or drink, absorb food and defecate)
- Fluid balance and the renal function (ability to pass urine in adequate amounts)
- Occurrence of any abnormal losses
- Bowel movement
The amount of fluid required by a person and the urine output varies with age, weight, activity and physical surrounding.
The water intake of a 50-90 kg adult person is about 2500 to 3000 ml per day or 2 ml/kg/hour. Normally, this is accomplished by:
- Water consumed as drinks (usually about 2000 ml)
- Water that is part of solid food
- Water produced in the body as a product of metabolism
The greater part of this water is re-excreted as urine, the amount of which can be measured by various means. Urine output in an adult is between 1000 to 1500 ml per day.
Another normal means of output of water is through evaporation of water from the skin and mucous membranes (mouth, throat, respiratory tract) and also through sweating. The amount contributed by these two mechanisms is about 800-1200 ml (dependent on climate and environment). In clinical practice, this amount is not measurable and is called the insensible loss (actually it is the loss not measured).
The amount excreted as urine and that by insensible loss added together balances with the normal intake. If there is more loss, due to either higher temperature of the environment or the person’s body, then the amount of urine output is expected to be less.
Some 300 ml of water is also excreted together with faeces and is also not usually measured. In cases of diarrhea, significant amount of fluid may be lost with the stool. The frequency of defecation also can provide an indication of bowel movement.
Structure and Content of the Intake-Output Chart
When providing and monitoring fluid intake and output, clinical care providers use two types of forms/charts, one for purposes of planning and the other for recording findings. Each type consists of different components as shown below:
- The Plan (the intended amount to be given as ordered)
- Type of fluid
- The amount intended for a given period
- Other electrolyte or drug to be added
- The Record or result
- Intake – actual amount administered or taken
- Output – amount of output that can be measured
- Fluid Balance
Sometimes the nature of the fluid output (colour, turbidity etc.) and the occurrence the passage of stool by the patient may be noted. The nature of the stool (consistency, colour) may also be indicated.
Transferring the Order/Plan to the I-O Chart
The order itself is often written in the continuation sheet of the Medical Record as part of the treatment plan.
Normally, nurses copy the orders into another sheet and converts it into a plan used as a guide to administer the infusion. For intravenous (IV) fluid therapy, it would be better if the doctor him/herself can write the plan and brief the nurse regarding the plans rather than just placing an order. For enteral feeds, because of the methods involved, it is easier for the doctor or dietitian to just order and for the nurse to plan the route, intervals, frequency and rate.
The plan is often attached to the I-O chart both of which are placed together with the nursing observation chart usually clipped on to a clip-board or a file separate from the medical record. The information is then recopied into the I-O chart. The beauty of the paper-based I-O chart is that it is very concise, providing a lot of required information on a single chart.
How the data is transferred from the order to the plan and then onto the chart will be discussed later.
Providing Fluid by the Intravenous (IV) Route
The Plan for Providing Fluid by the IV Route: The Fluid Regime or Orders
When IV fluid is to be given, the recommended fluid intake is usually ordered by doctors.
The order for the type and amount of fluid to be infused is called the Fluid Regime.
It is routine for doctors to order IV fluids to meet the needs of a 24 hour period. Strictly, doctors should order IV fluids for the duration that they are required. When fluid is ordered for resuscitation, it is ordered only for the period required to achieve stabilization. The regime is then reviewed taking into consideration the change in the patient’s condition. Also, a review is done if there is an order for the transfusion of blood or an order for administering drugs diluted in a considerable amount of IV fluid.
The doctor is often guided by normal daily (24 hour) requirements and the estimated fluid deficit. This period varies with the time of admission of the patient. Therefore, IV infusion can be started at any time of the day and may be extended beyond the 24 hour nursing shift. This does not matter because IV infusion is meant to be continuous. The nurse, may write a plan that extends to the next working day but it is probably better to write a separate plan for the shifts of current nursing work day and another for the shifts that follows.
Periods In Intake Output Planning and Charting
There is a need for greater clarity in ordering the fluid therapy regimen. Some methods that is still in practice can lead to confusion.
Common but Incorrect Way of Ordering IV Fluid Therapy
Writing an order in this way is not advisable because it relies too much on nurses to:
- Understand the order,
- Arrange the sequence of the type of fluids and
- Calculate the amount to administer for a given period
The nurse would probably calculate the rate as 2500 divided by 24 hours (one bottle or pack taken to be 500 ml). She would most likely give all 1500 ml of Dextrose 5% first before giving the 1000 ml of Normal saline. On the contrary, the doctor probably hoped that she will start with Normal saline and the alternate with Dextrose 5%. The assumption is also made that the nurse knows she should add only 1 gm of KCL per 500 ml of fluid. A better but still incorrect way is to order is as below.
Better but Still Incorrect Way of Ordering IV Fluid with Addition of KCl
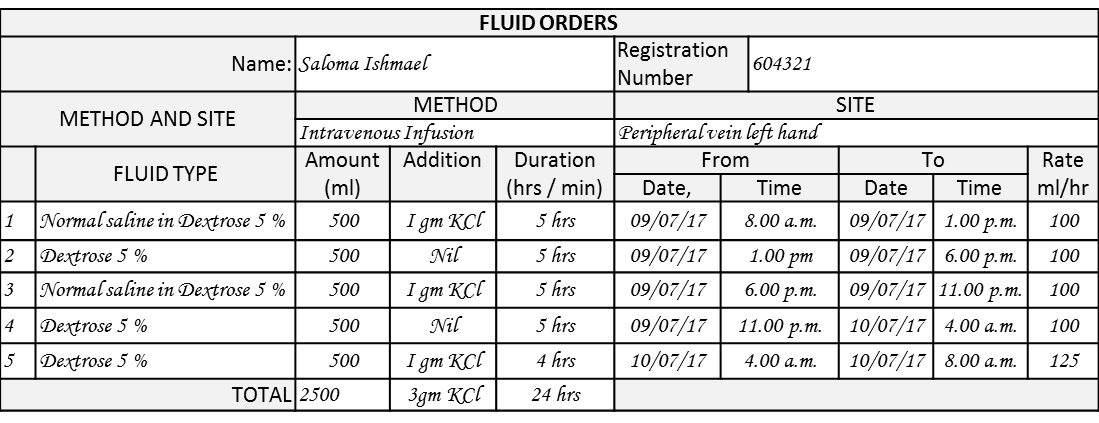
Proper IV Fluid Order and Plan
A proper IV fluid order would indicate the type of fluid to be given, the starting time, the period it is to be administered. When properly written it also acts as the plan. It is important that the doctor prescribes the type of fluid to be given, the amount of each type, the total amount for period and the route / site planned. It would mean that the order and plan is written on the same form. The nurse needs only to calculate the rate. This arrangement is subject to policies of the hospital concerned.
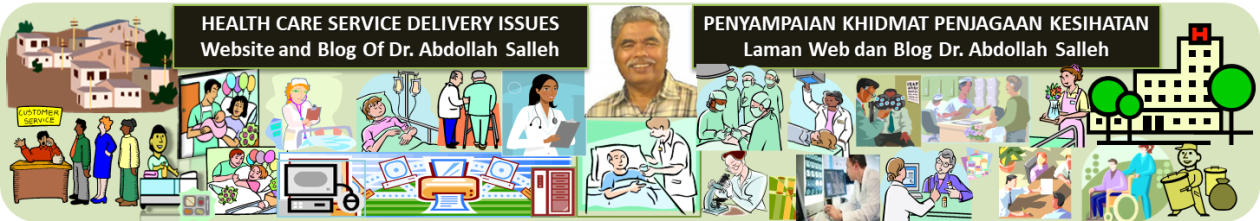
Giving IV Infusion of Only One Type of Fluid via a Single Vein
Frequently, fluid is given via one infusion set into a single peripheral or central vein. For providing the normal requirements for water, it is common practice to order 1/5 Normal saline in Dextrose 5 % at a rate that will provide the volume and sodium required (in both adults and children). For total parenteral nutrition, fluid containing all the necessary nutrients including electrolytes may be given from one bag. The total volume to be given is determined and the rate calculated.
While the doctor may order the total volume for a 24 hour period, the nurse need to take into consideration how the fluid is to be provided. She/he will need to plan the amount, duration and when the bottles/bags needs to be changed. Then, she/he needs to calculate the rate of infusion in ml/min and the equivalent drops per minute if a gravity driven drip set is used rather than an IV infusion pump.
Plan for IV Infusion if Only One Type of Fluid is to be Given
However, if additions are to made then the amount to be added and to which bottle/bag needs to be indicated.
The period of infusion can be extended to the next day i.e. beyond 24 hours but when the intake is measured and totaled it would be for the three nursing shifts.
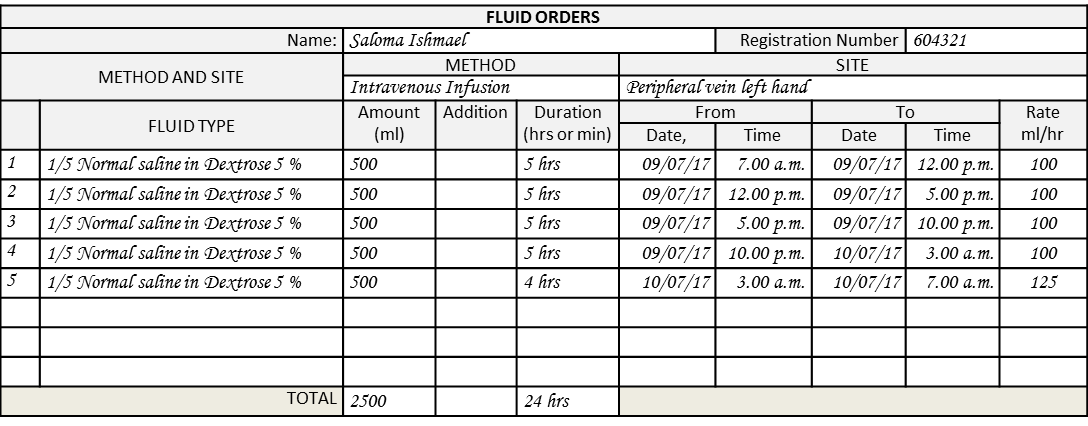
Giving More than One Type of IV Fluid via a Single Vein
Often, different types of fluids are ordered to be given sequentially, through a single vein. These may include blood, plasma, plasma substitutes, albumin etc. The doctor needs to indicate clearly the sequence and duration of infusion of each pack/bottle of fluid as well as any additions to be made to each of them. In effect the doctor writes the plan. The rate may be calculated by the nurse.
Order and Plan for Infusion of IV Fluids if More than One Type of Fluid is to be Given
In this example, the doctor intends to give the patient 2500 ml of fluid (the normal daily requirement) in 24 hours. He/she would like ensure that the patient is given 154 meq of Na and 39 meq of K+. Therefore, he/she has ordered 1000 ml of 0.9% Sodium Chloride in 5% Dextrose. He/she has also indicated that 1 gm of KCl is to be added to three (3) of the solution bags ordered.
In practice, KCl may be supplied by the pharmacy in gm per vial (usually 1 gm per vial equivalent to 13 mEq) or in meq per vial (usually 10 mEq per vial). KCl is a dangerous drug and should be ordered with care.
If fluid is to be given using more than one method or via more than one site then the order should be documented on a slightly different type of form.
Giving IV infusion at More than One Site
There are instances when more than one IV infusion site is used i.e. either:
- A peripheral vein plus a central vein
- More than one peripheral vein
The circumstance is also similar when two IV infusion sets/line are set up to run through one vein (piggy-backed) to give a different type of fluid e.g. diluted medication. The orders should be made on a chart specially designed for the purpose.
Piggy Backed IV line

For this purpose, the type of chart used has separate sections for different sites so that the specific site (vein) the fluid is to be infused is specified. Fluid may be given also via an arterial line to keep it patent. In children, this amount is significant enough to be recorded.
If there are more than one line, attached to a vein then the line need to be named.
In the example below, the doctor provides a total of 3000 ml of IV fluid consisting of 2000 ml of Total Parenteral Nutrition Solution (in one bag) via the Central venous line and 1000 ml (in two 500 ml bags) of Normal saline with 2 gm of potassium added in each bag to offset for dehydration, hyponatraemia and hypokalaemia in the patient.
Order and Plan if IV Infusion is to be Given at More than One IV Site
The above form may be used for ordering and planning for infusion via a different set piggy-backed to the first set.
Order and Plan if IV Infusion is to Be Given Using More Than One Mode
There are instances when fluid is given via more than one mode i.e. via the intravenous route and also one of the enteral routes. The same form for ordering and planning as shown above may be used. The type and amount of fluid to be given using the different method at the different the site is written on the separate section.
Relationship between Plan and Intake Chart
Data from the plan is need to be accurately transferred to the chart by handwriting. It is a good practice to have the plan and chart together in one place e.g. on a clip-board or in a file.
Transfer of Data from Plan to Intake Chart
Monitoring Intake
In the clinical setting, the type and amount of fluid whether given parenterally or enterally, needs to be measured. The type of fluid is copied from the plan.
When fluid is given via intravenous (IV) infusion, the amount of intake is taken as the amount put up minus the amount left over. When an infusion pump is used, the volume is calculated by the machine based on the flow rate set by the nurse.
How fluid is measured, when given through the enteral route, depends on whether it is given by intermittent bolus feeding or continuous infusion driven by either gravity drip or by the use of an infusion pump (will be discussed later).
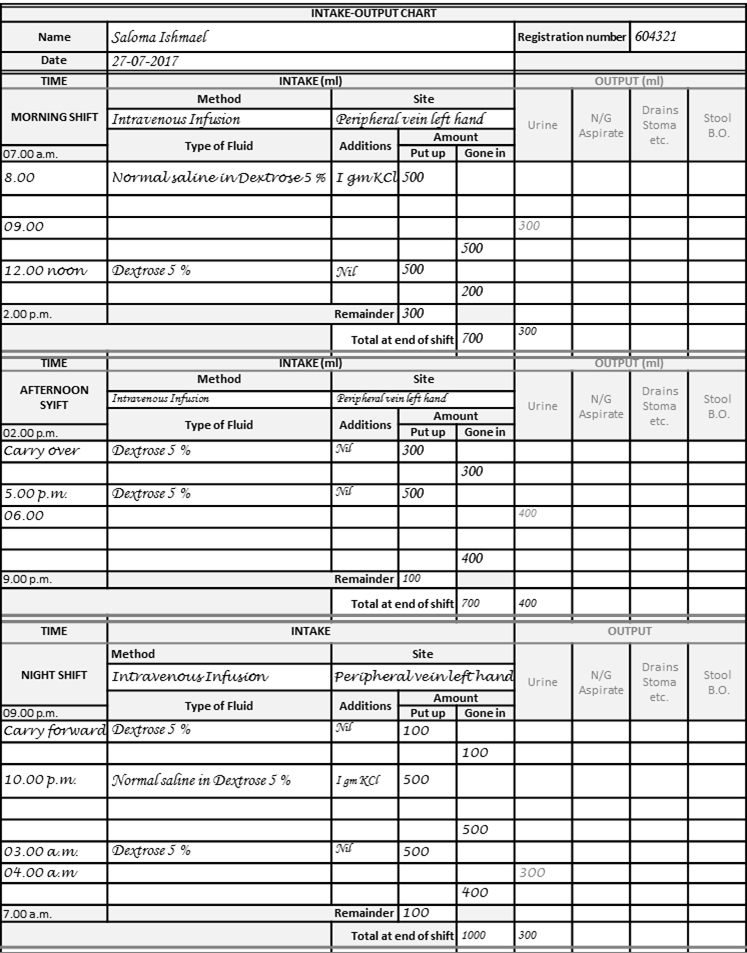
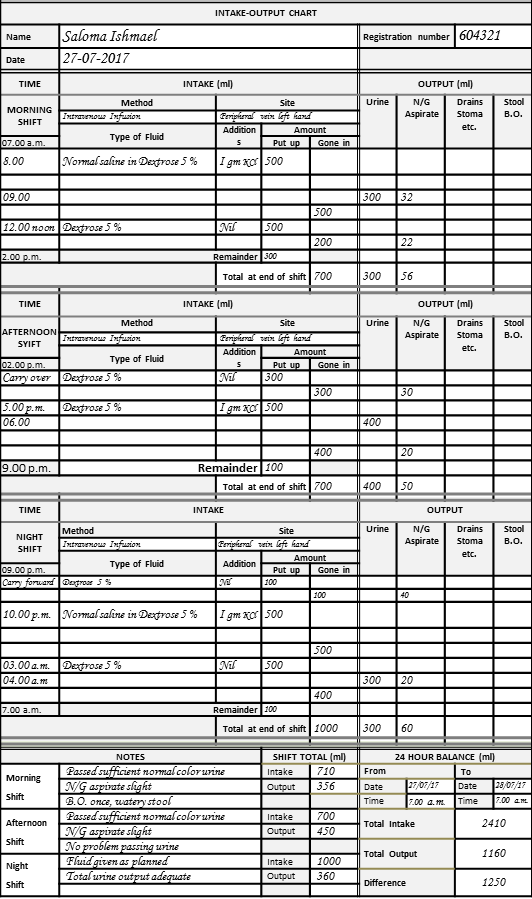
Structure of Intake Output Chart
The Intake-Output chart is so named because on one side is the Intake and the other the Output. Measurements of volume are in ml. The chart is for a 24 hour period but, for practical reasons, it does not follow the calendar day (i.e. is not from 12 Midnight to 12 Midnight of the next day). Rather, it follows the nursing shift i.e. usually from 7 a.m. on the starting day to 7 a.m. the next day.
While the order or plan may extend into the nursing morning shift of the next day, the intake and output measurements end with the night shift. Charting is then started on a new form.
A common Intake-Output Chart is used for when fluid is given intravenously as well as by the enteral routes. Also, the same chart is used to enter data and to view what has been recorded.
The chart is a table where the rows divide the chart into time intervals.
The columns indicate:
- the type and amount of the fluid that has been given and
- the mode and site of administration
- the fluid output including urine, discharges or drainage.
(The structure of the Electronic order form and Intake Output Chart for a computerized Clinical Information System is discussed in another paper yet to be written).
Normally the empty chart is pre-printed and the data is entered in ink. Charts are usually single sheets of standard A4 paper and are often separated from the main medical record e.g. placed on a clip board. There is a danger of losing the identity of the patient whose I-O is being charted. It is important to document the Name of the Patient, the Registration number / Medical record number and the (starting) date for which the chart is used. At the end of the patient’s stay, the charts should be reincorporated as part of the Medical record.
All relevant particulars of the input and output data are charted in the appropriate time-interval (period) on the chart under the relevant the chart headings (column and row titles). The amount of both the input and the output is totalled for every shift (sub-total) and for the 24 hr period (grand total) starting at 7.00 a.m. and ending at 6.59 a.m. the next day.
Monitoring Intake when Fluid Is Given via Intravenous Infusion
The chart is designed to follow the process of giving intravenous infusion. After receiving orders from the doctor on the regimen to be followed, the nurse obtains the first IV Fluid pack/bottle of the specified type from the pharmacy or floor stock. Where the fluid solution is sourced or kept from depends on policy. It is very convenient for IV drip solutions to be kept as part of the ward stock, because large amounts are used especially in acute care wards. However, issues arise when additions like electrolyte such as Potassium or drugs such as inotropes (dopamine, dobutamine), heparin and antibiotics need to be added. Hence, the admixture may be done by the nurse in the ward or by pharmacists.
Currently, many hospitals give to nurses the responsibility of mixing common substances to fluids in packs/bottles. The nurses are trained on how to ensure that the right concentration is given and the aseptic technique is followed.
The need for mixing to the correct concentration and asepsis is also applicable if pharmacists are to make the additions. The advantage is less people need to be trained. The trade-off is that the supply may be delayed. The workload of the pharmacy will be increased and the staff available may not be able to cope. However, most hospitals make it a rule that only pharmacists are allowed to mix items such as parenteral nutrition and cytotoxic drugs.
The workflow for starting and recording IV infusion is as shown below:
Workflow Chart for Starting and Recording IV Infusion by Nurse Using Ward Stock
Entering Data into the Intake Chart
The instances when the nurse needs to enter (write down) data into the chart include:
- At the beginning of putting up an IV infusion
- At the beginning of a shift
- Whenever a pack is finished and another is put up
- Whenever the regime is changed
Recording of Time
The nurse enters the actual time that she starts the infusion rather than the time planned. The time is recorded on rows within the column on the extreme left. The same column is use for all activities and happenings including for the output (e.g. the time when the urine is collected). The time fluid is put up need to be recorded. However, the finish time need not be recorded; assuming that in a continuous infusion, after the last pack/bottle finishes. the next one is put up immediately.
Recording of Amount of Fluid Put Up
At the beginning, the nurse records the following data in the Intake Chart:
- The time the infusion is started
- The type of fluid being set up
- The amount set up
The nurse needs to ensure that the type of fluid being infused is the same as the one ordered. This is done by confirming with the particulars on the label of the pack/bottle. The type of fluid being set up (e.g. Normal saline, Dextrose 5%, Normal Saline in Dextrose 5% or parenteral nutrition solution) is then recorded. Because the columns may not be wide enough, it may be necessary to use abbreviations.
The amount of fluid put up is the amount in the pack/bottle or the chamber if a set with a chamber is used (as in paediatric cases). The chamber usually contains the maximum of 100 ml. If a syringe is used with a pump, then the amount set up would be the amount drawn into the syringe (usually 50 or 100 ml).
If additions are made then she/he needs to make a note on the existing label or by sticking another label on the pack/bottle. The rate of infusion may be decided in the fluid intake / infusion plan. A good method is to indicate the additions, the rate and period it is to be completed on an extra label stuck to the pack/bottle. In the example below, instruction is given at rate of 100 ml/hr. to finish the 500 ml bottle at 12 noon.
Instructions on Extra Label on the Pack/bottle

Where IV infusion has been started on a previous shift, the nurse would record the amount of fluid left in the pack/bottle as the amount carried over. If the pack is finished in the middle of the shift, the volume in the replacement pack is recorded as the amount set up.
Recording Amount of Fluid Infused (Gone In)
If the fluid flow is by gravity and the flow rate is controlled by a flow regulator (in drops/min), then the amount infused is calculated as amount set up minus the amount left in the pack. The amount that has gone in need to be recorded at these instances:
- When the pack/bottle is finished in the middle of the shift,
- At the end of the shift
The amount gone in at the end of the shift is calculated by subtracting the remainder from the amount set up or remaining in the bag/bottle at the beginning of the shift. The amount of the remainder fluid is noted in the chart for the benefit of the nurse of the next shift.
If an infusion pump is used, the amount given as indicated on the machine is read from it. Even though it is not necessary to know the amount left behind for purpose of calculation, it is good practice to make a note of the remainder left in the pack/bottle. Also, if a change is made, the new type of fluid and the amount put up must be recorded
Since the amount that has gone in is for a period, the data must be written at the time it is calculated or read i.e. on another row on the Intake Chart and not on the same row as the time it is put up.
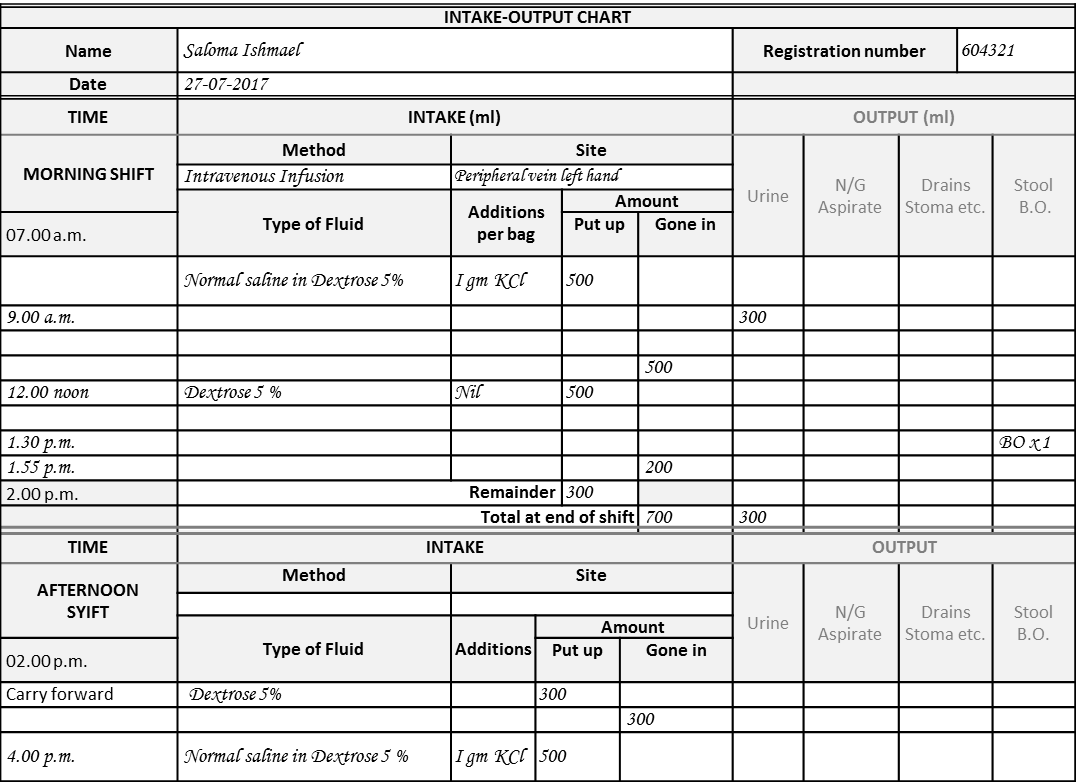
Chart for Single IV Site or Single Method of Providing Fluids
It is quite common for patients to be given intravenous fluid therapy. Frequently, IV fluids are given via a single vein using a single set. The chart used for this purpose is as shown below:
Paper-based IV Fluid Intake Chart for Single IV Site
Setting and Controlling the Rate to Ensure the Correct Amount Is Given
When a certain amount is planned for a period, e.g. 24 hours, the nurse must ensure that the rate of flow is set so that the intended amount will be infused. If the infusion time is delayed or brought forward for any reason, then the rate need to be increased or decreased accordingly so as to ensure the necessary amount is in fact transfused. Therefore, the nurse needs to observe (by counting or otherwise) the rate of flow and the remainder amount in the pack. Often, the right amount is not given if the line is obstructed or the rate becomes too fast.
In emergency situations when fluid is given rapidly, the nurse ensures that the actual amount required as ordered is given at the speed required. It may be beneficial to record the amount every hour in the amount “gone in” column.
Cumulative Total at the End of Each Shift
Since, traditionally, the recording the intake and output is the duty of nurses, it is logical that the chart is segmented into sections according to nursing shifts.
- Morning shift: 7.00 a.m. to 2.00 p.m
- Afternoon shift: 2.00 p.m. to 9.00 p.m.
- Night shift: 9.00 p.m. to 7.00 a.m. next day
The nurse on duty calculates the cumulative total at the end of the shift. The remainder or amount left-over of any IV fluid or enteral fluid in the container is noted to be carried forward to the next shift in the “remainder” column.
The remainder will be recorded again by the nurse in charge at the next shift as the starting amount. She/he notes this as being “carried over”.
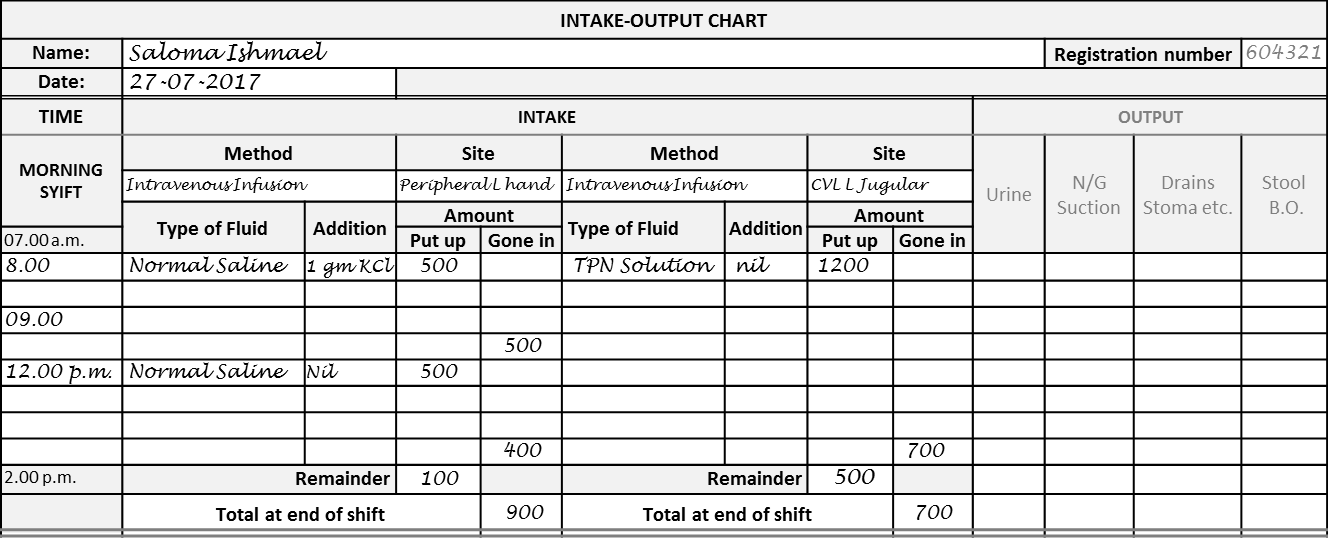
Charting Intake when Fluid is Given by IV Route Using Two or More IV lines
Two alternative approaches can be taken in this situation:
- Use two charts
- Use chart with two sections
Use of Two Charts
To record the intake two separate charts may be used for the each of the line. The shift total is made up by adding the total for each line. However to avoid confusion, for recording of the Output only on one of the charts should be used (preferably the second one).
Use of Chart with Two Sections
A different Intake Chart with two sections can be used when two sets of infusion system are used for e.g.:
- to infuse fluids into two separate veins, or
- a second set is piggy backed to a line on the same vein,
It caters for the different site of administration by having two sections for intake as shown below:
Chart with Sections for Two Sites of Administration (for one shift)
In this chart, the width of the column is compromised and abbreviations may be used. It is quite impossible to have charts with columns for more than two sites or routes. In this situation, it is better to use more than one chart.
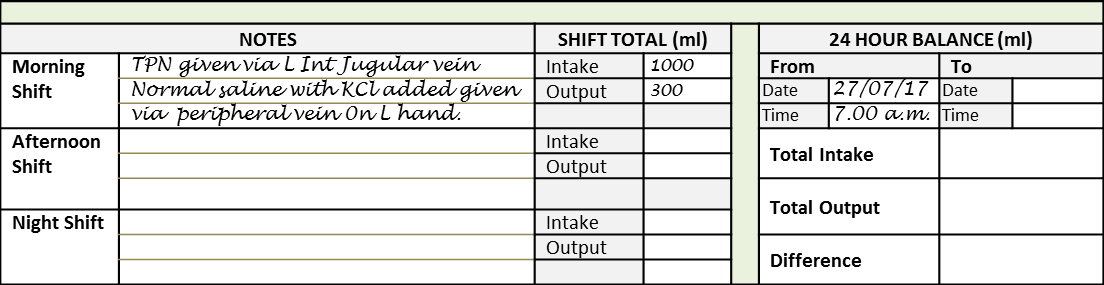
Shift Total When More than One IV Site is Used
When two separate charts or a chart with two sections are used, the total for each section is added to give the shift total. This is recorded at a supplementary section at the bottom of one of the charts preferably the one that comes later.
Shift Total When Fluid is Given by Both Central and Peripheral Veins
Providing Fluid through the Enteral Route
Plan for Providing Fluid through Enteral Feeds
The doctor or nurse may order and plan the feeding regime or a dietitian is consulted. The dietitian may recommend the type and amount of liquid food formulation to use based on fluid and calorie requirements. Usually, the nurse will plan the frequency of feeds and the amount for each feed.
Enteral tube feeds may be given in two ways:
- Intermittent bolus feeding
- Continuous Infusion via an infusion set attached to the tube with the flow determined by gravity or using an infusion machine
Providing Fluid Input via Mouth
For patients taking well orally and on a normal diet, an Intake-Output Chart is quite unnecessary. It is only in situations where there is clear indication that the patient’s oral intake needs to be monitored and controlled that an I-O chart is indicated. Indications include:
- When there is doubt regarding ability of the patient to take adequate amounts of fluid
- Whenever the patient is given fluids orally in addition to IV fluids
For oral feeds, depending on circumstances, the doctor or nurse may decides on how much fluid to be given and how frequently. The nurse provides the desired amount to the patient in a container (e.g. cup, glass or bowl) and record this as ‘amount supplied’. She/he then records the amount that the patient actually takes.
Situations where the amount needs to be controlled and measured carefully are:
- Patients on trial of oral feeding after prolonged period of IV Therapy (e.g. after aesophageal, gastric and intestinal surgery)
- Patients reluctant to take orally (due to anorexia etc.)
- Patients where intake needs to be limited (e.g. renal failure)
Providing Feeds via Nasogastric and Nasoduodenal / Jejunal Tubes
Enteral feeds may be given in two ways:
- Intermittent bolus feeding
- Continuous Infusion via tube with the flow determined by gravity or using an infusion machine
Intermittent Bolus Feeding
Intermittent bolus feeding is suitable mainly for feeds via nasogastric tube or gastrostomy, even though it is also practiced for feeding via nasoduodenal or nasojejunal tubes. The nurse introduces the amount planned but it is recommended that she/he aspirates the stomach contents, before the next feed, to determine if the feeds has been passed on and not retained. If some amount is retained, she would then have to subtract this from the amount introduced and record the resultant amount as ‘amount given’. If all or most of the feed is not passed on or retained, this will indicate that there is problem with gut motility or absorption. The route of administration may be reduced in amount, a different type of formula or feeding by this route is abandoned,
Enteral Feeding via Continuous Infusion
Bolus feeding may give rise to the problems of inadequate digestion and diarrhea. By giving feeds in small amounts there is a better chance of absorption and less chance of food left undigested. The incidence of diarrhea is also reduced. The setting up, calculation of rate of infusion and recording amount gone in and left over is similar to that of IV infusion.
Feeding via Nasogastric Tubes
Feeding can be given via a nasogastric tube as a temporary measure in the situation where a patient cannot swallow. For feeding for longer periods, creating a gastrostomy for the purpose is better. Usually, the intermittent bolus feeding method is used for this route.
Feeding via a Gastrostomy
A gastrostomy is done to bypass the mouth and esophagus in cases of inability to swallow, obstruction or injury to the aesophagus. If the rest of the gastrointestinal tract is healthy, blended or homogenized food of any type can be given. Where the rest of the bowel has limitations in motility or absorption, then milk and other formulas may be given. The intermittent bolus feeding method usually works well for gastrostomy feeding.
Gastrostomy Tube
Feeding via Nasoduodenal or Nasojejunal Tubes
A fine (small diameter) feeding tube can be placed so that it ends in the duodenum or jejunum using endoscopy or radiology imaging. It is indicated when there is gastric stasis or risk of aspiration as well as for acute pancreatitis and hyperemesis. Feeds via these routes are administered continuously by infusion pump. The initial rate of administration is increased gradually and is combined initially with parenteral nutrition achieve the necessary caloric intake. The type of feed is similar to that of jejunostomy feeding.
Feeding via Jejunostomy
Depending on the ability of the jejunum and ileum to pass on and absorb liquid food , three types of liquid formulations may be given:
- Standard Formula i.e. Liquid formulations of protein, sugar and fat usually milk-based
- Elemental Formula these are usually proprietary formulas where food substances supplied are those that are broken down into simple elements which are easily absorbed (protein in the form of amino acids, , sugar as glucose or dextrose and fat as fatty acids).
- Special formulas that are elemental formulas with some elements increased or added or reduced or removed. The content of the formulations depends on the types of disease.
Jejunostomy feeds are best given by continuous infusion either via:
- Gravity driven drips via closed administration sets
- Enteral feeding pumps
Orders and Plan for Enteral Feeds
Orders for Nasogastric and Gastrostomy Feeds by Doctor or Dietitian
The doctor or dietitian needs to specify the type and amount of feed for the day. The frequency of feeding is best left to the discretion of the nurse
Orders for Nasoduodenal, Nasojejunal and Jejunostomy Feeds by Doctor or Dietitian
These feeds need to be given via continuous infusion. The order should specify the amount and type of feed. The frequency, periods of delivery and rest are usually planned by nurses.
Orders Jejunostomy Feeds by Doctor or Dietitian

(click on image to enlarge)
This order can easily be written as: “to give 2400 ml of enteral feeding formula via jejunostomy in 24 hours using infusion pump”.
Plan for Enteral Feeds
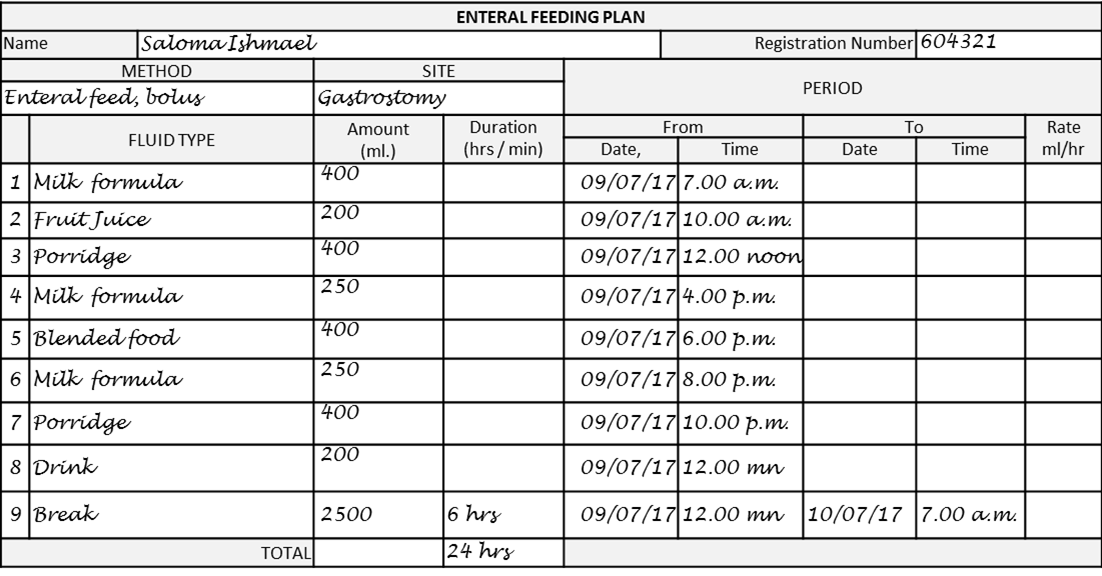
Plan for Nasogastric or Gastrostomy Feeds
Feeds via gastrostomy and nasogastric tubes are usually given by intermittent bolus method. For nasogastric feeding it is better to use only milk formulas. For gastrostomy, as the tubes are much bigger, blended or liquid mixtures such porridge or soups can be given. The time of feed is indicated but since it is to be given as a bolus it is not necessary to indicate the period. In between feeds, the tube is closed with a spigot and patients can move about if they are able to. The plan also acts as an order to the unit supplying the feeds (e.g. the kitchen).
Plan for Gastrostomy Feeds (example)
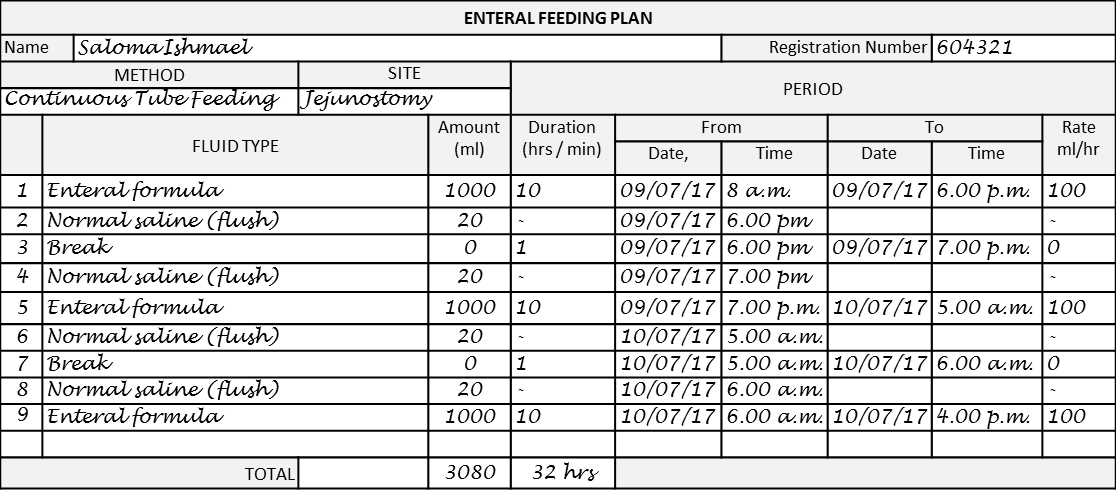
Plan for Enteral Feeding by Continuous Tube Feeding
In order to avoid physiological complications, Nasoduodenal, Nasojejunal and Jejunostomy feeds are best given via continuous infusion using infusion pumps. It is also good to have a break and stop infusion for a short period to give the intestine some rest. It is also good practice to clear the tubes with water or saline from time to time. The tube has a side connection for this purpose.

The plan can be written by doctors or dietitians. However, it may be better to leave it to nurses because they have better knowledge and skills on the techniques. They would also prefer to determine the periods of feeding rest and clearance of the tubes.
Enteral feed formulas used for continuous infusion usually comes as sterile solutions in 1000 ml bottles. To meet the daily fluid and calorie requirements of adults 2500 ml (two and a half bottles may be required). Hence, the plan may be extended to the next working day to finish the third bottle (unless a 500 ml bottle is available). In this way the remainder in the bottle/container is used for the next shift and not wasted.
Plan for Continuous Jejunostomy Tube Feeding (example)
Monitoring Intake of Fluid Given by Enteral Route
Use of Chart
It is best that the same Intake-Output Chart is used for when fluid is given either via the intravenous or enteral route.
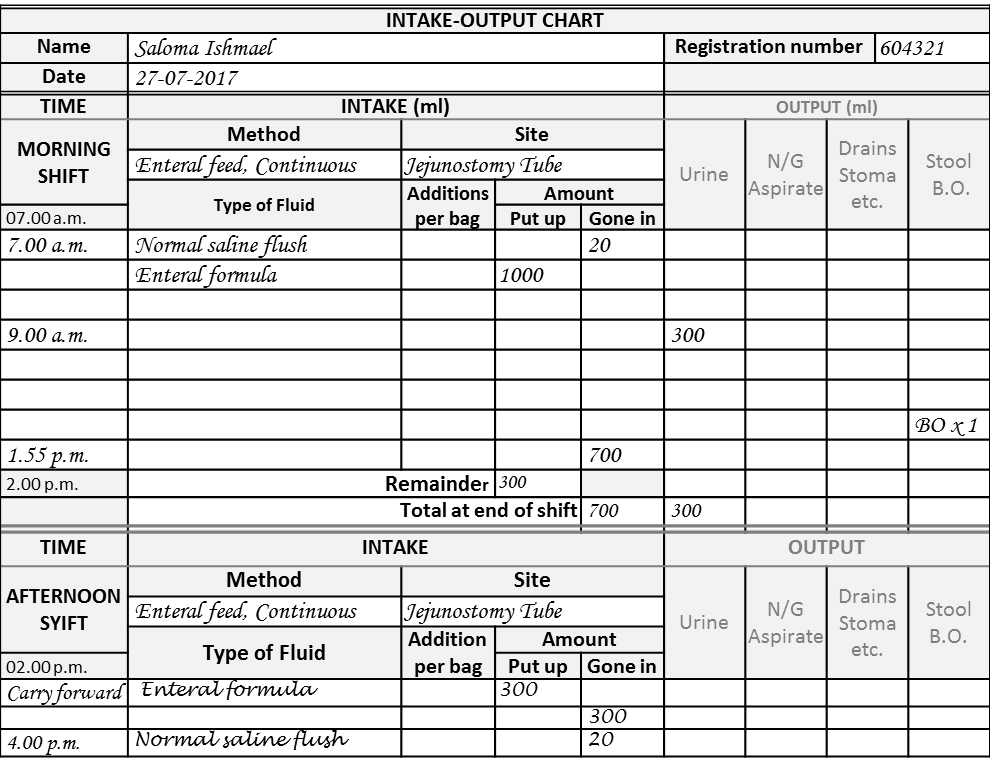
Recording Intake of Fluid Given via Gastrostomy by Bolus Feed
Since the feed is given bolus only the time rather than the period need to be recorded.
Recording Intake of Fluid Given via Gastrostomy
Charting of Intake of Fluid Given by Continuous Enteral Feeding
The charting of intake of fluid given by continuous enteral feeding (i.e. via naso-dudenal, nasojejunal, jejuostomy tubes) is quite similar to that of intravenous infusion.
Recording Intake of Fluid Given by Continuous Feeding via Entrostomy
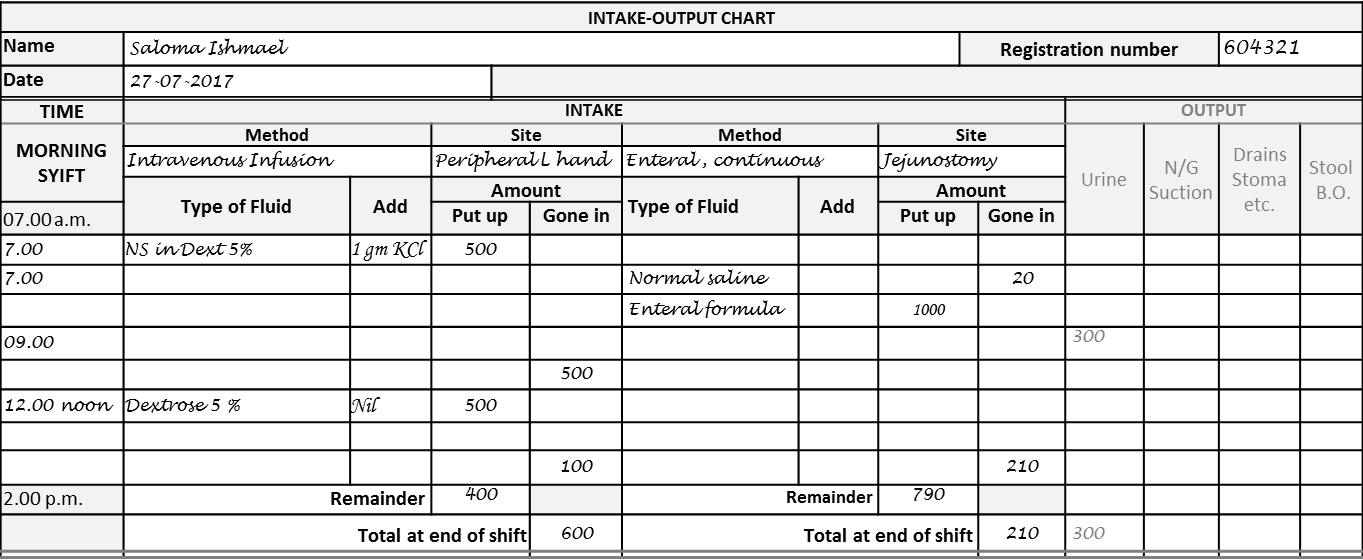
Charting Intake when Fluid is Given by More than One Method
There are instances when fluid is given by both IV and enteral route.
Two approaches can be taken in this siuation (just as for when fluid is given via two IV sites)
- Use two charts
- Use chart with two sections
Use of Two Charts
Two separate charts may be used one for each of the route/mode. The shift total is made up by adding the total for each route/mode. However to avoid confusion, for recording of the Output only on one of the charts should be used (preferably the second one).
Use of Chart with Two Sections
The Intake Chart with two sections can be used when two routes/modes are used. An example is when starting a trial of enteral feeding, the enteral feed is given at a slow rate e.g. 30 ml/hour while the rest of the fluid is given by the intravenous route.
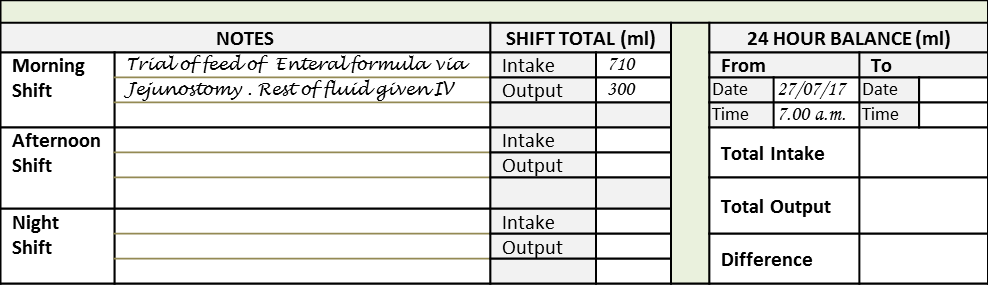
Charting Intake when Fluid Is Given by Both IV and also Enteral Route
Shift Total When More than One Route or Site is Used
When two main sections are used, the total for each section is added to give the shift total. This is recorded at a supplementary section at the bottom of the chart.
Shift Total When More than One Route is Used
Measuring and Recording Output
In the clinical setting, the normal output can be measured only partially. It is mainly a measure of the urine output. This amounts to 1000-1500 ml per day in a normal adult. Sometimes, especially in children the amount of loss due to diarrhoea is estimated. The loss from sweating and evaporation (insensible loss) is not measured. This is around 1000 ml. Hence, in a normal person the measured input is more than the measured output by around 1000 ml. This is not a deficit because it is not an abnormal loss.
Abnormal losses occur in situations where the patient has:
- A fistula originating from the jejunum or ileum
- An ileostomy
- A draining tube inserted into a body cavity containing fluid
Measuring Urine Output
When there is a necessity to chart the patient’s fluid balance, the urine is collected and measured. In a patient who is alert and not on a urinary drainage catheter, the patient or care giver collects the urine in a urinal or bottle each time urine is passed. The amount is usually measured by a nurse or nursing aid using a measuring jug and recorded on the chart. Dependable patients may also be allowed to measure the urine and record them on a slip of paper before recording them. The nurse copies the amount onto the I-O chart.
Urine output may need to be measured at the end of a shift or more often (e.g. hourly). Currently, the urinary catheter is attached through into a collapsible plastic with markings. The amount can be read from these markings or by emptying the entire content of the bag into a measuring jug when it is full or at the end of the shift or day.
If it is desirable to let the urine accumulate for the whole day, the nurse reads off the amount from markings (level in ml) on the bag and record this and the time in the I-O chart. To enable her to make the next reading, she may indicate the level at which last measurement was made – on the bag with a marker or tape. Otherwise, she can also subtract the reading of the previous level from the level at the time of the current reading. This gives the amount passed between the times of the two readings. If the urine bag is full, the urine is discarded and the amount recorded.
If urine output is to be measured hourly, then the use of the standard I-O chart may not be suitable (too many rows required). The output may be recorded on a separate chart and then the total for a shift inserted into the main (standard) chart.
Measuring Other Losses
Measuring Losses from Drainage Tubes
Patient who has a collection of fluid in a body cavity (like in pleural effusion or ascites) may have a drainage tube inserted into the cavity to drain the fluid. After surgical operations, drains may be inserted into abdominal or thoracic cavity and abscess or cyst cavities to facilitate drainage of secretions or discharges such as blood, serum or pus.
To measure the loss, one method is to read from markings on drainage bags / bottles. After reading the loss for the current period, she may use an ink marker or tape to indicate on the bag or bottle the level when it was last read. The amount at the end of a shift is calculated by subtracting the amount of the previous reading from the accumulated amount.
Making Markings on Drainage Bottle
In the second method, reading is done and then the whole bag or bottle is emptied. In a closed drainage system changing the whole drainage bag/bottle at every shift is not done. But it is indicated if the bag or bottle is full.
Emptying a Drainage Bottle
Other forms of fluid or semi-fluid may be discharged by the body. These include
- Intestinal contents
- Gastric juice from a nasogastric tube
- Urine from a nephrostomy tube
If the patient has a fistula originating from the jejunum or ileum, the intestinal contents are collected into a jejunostomy or ileostomy bags. Measurement of the output is made by transferring the content into a measuring–container or aspirated with a syringe.
Data Entered for the Output
The type of fluid that is excreted or drained out is indicated by the headings on separate columns. These include:
- Urine
- Nasogastric aspirate
- Drainage from drainage tubes, stomas etc.
- Stool/faeces (only the occurrence of passage of stool is recorded. In children with diarrhoea the loss may be measured)
The time of measurement for each output is written on a separate row unless it coincides with the time when the input was recorded. There should be enough rows on the chart to record the time of intake as well as output.
Each type of output has its own column title. As space is limited, total volume of all types of output of each shift needs to be added and written at the bottom of the chart (see below).
Entering Data for Output (Morning Shift)
Total Output at the End of the Shift

Fluid Balance and Interpretation of Intake-Output Chart
Interpretation of the Fluid Balance
Losses: Urine
Urine, though an output, is not normally considered as a loss because urine production is a normal mechanism for the excretion of products of metabolism. In normal circumstances, if too much urine is produced the commonest reason is that more fluid than what is required has been given to the patient. The intake therefore needs to be reduced. A common mistake is to increase the intake to catch up with the urine output.
However, the clinician needs to be aware of circumstances where an abnormal amount of urine is excreted because of complications of disease for example
- osmotic diuresis
- diabetes insipidus
- high output renal failure
Drainage as a Loss
The doctor need to determine whether the drainage constitutes an active loss or drainage of accumulated fluid for which the body has been compensated. Fluid in ascites or pleural effusion usually had accumulated for some time and it is wise not to replace it volume for volume. However if there is re-accumulation after the initial drainage, it may have to be replaced.
In intestinal obstruction fluid may well up into the stomach and the volume Nasogastric aspirate will rise. It is quite common practice to replace it volume for volume with IV Normal-saline. However, it must be remembered that most of the accumulation is in the small intestine. Therefore just replacing the Nasogastric aspirate is not enough. Judgment on the fluid need must be based on the diminishing urine output, increased pulse rate and drop in blood pressure.
Summary
In the monitoring of Intake and output the following need to be taken into consideration:
- There should be an order, a plan besides the recording of fluid intake and output.
- Sometimes it is best to combine the order with the plan
- Orders and plans must be for a defined period
- The measurement and charting of Intake and Output follows the Nursing shift.
- Mode/route and site of administration should be indicated.
- Measurements should be as accurate as possible.
- A good part of losses are not measured. Therefore the amount of intake compared to the output as per the I-O chart is not supposed to be balanced.
- Besides the I-O chart, other clinical factors should be considered when fluid therapy is planned.
Entire Completed Intake–Output Chart
Entire Blank Intake–Output Chart
Link to MSWord version of Chart
INTAKE-OUTPUT CHART MS Word Version
References: