Date First Published: July 24, 2014
Date Last Revised: March 4, 2018
PATIENT MANAGEMENT SYSTEM (PMS)
COMPONENTS AND CHARACTERISTICS OF Patient Management System
The Patient Management System (PMS) or Patient Administration System consists of applications designed to enable service delivery managers and care providers to manage an individual or groups of patients as clients or customers in an efficient, responsive, flexible and customer-friendly manner with optimal use of resources. Indeed a better name for it would be the Client Management System but the terms mentioned above have gained popular use. The term ‘management’ here does not include the provision of services of looking after the patient’s health and illness. In that context the term ‘care’ is used.
The Patient Management System (PMS) has these components:
- Patient Registration Application
- Client-Resource Management
- Charging, Billing and Receipt of Payment System
The division of the system into various sub-systems and applications, listed below, are for the purpose of defining the scope. It would be preferable for these functionalities to be provided in a single integrated system with the exception of the Charging, Billing and Receipt of Payment where a third party application may be used if it is not already an integral part of the Patient Management System.
Relationships of the Patient Management System (PMS)


THE PATIENT REGISTRATION APPLICATION
The registry of clients or customers of a health care facility is managed through The Patient Registration Application. Registration itself has two purposes and is facilitated by two linked modules of the application i.e.:
- Client Registration
- Visit Registration
CLIENT REGISTRATION (Patient Master Index)
This application software is used to enlist a new person as a client (patient) of the healthcare institution. The functions include to:
- Capture identification and demographic data
- Create a new entity with a unique identification number in the Database of Patients
- Maintain a single Medical Record for the patient
- Maintain a master list of patients as a permanent register i.e. the Client Register also known as “Patient Register” or the “Master Patient Index” (PMI)
The identification number is a unique person identifier and which may also act as the Medical Record Number (MRN). It allows data regarding a single patient to be constituted as a single record, shared between systems and used for subsequent visits and encounters without the need for repeated data acquisition and entry of static data. Before giving the number it is essential that the patient is properly identified i.e. the patient is actually the person he/she claims to be. This is usually done by comparing with the identification data already available on his/her identity card/passport. The criteria for identification is matching appearance of the photo in the ID with the actual person plus his/her age, gender and ethnic origin. Biometrics may also be used. All these data are then inserted into the the Client Register also known as “Patient Register” or the “Patient Master Index” (PMI). A photograph of the patient is taken and kept in the patient database to identify him/her at subsequent visits. A search of the Patient Master Index is used to verify if a person is already a client of the hospital. A person should not appear twice in the index.
Other information regarding the client such as addresses, occupation, contact numbers etc. may be collected at the time of registration or subsequently. These data may vary and therefore is modifiable.
New born infants need to be registered in the same manner as other clients. In addition, certain additional information may need to be acquired for the purpose of birth registration.
A patient presenting him/herself at the reception counter may or my not be a registered client of the hospital or clinic. A search of his/her identifier (name, ID) in the Patient Master Index is used to verify if a person is already a client of the hospital. This ensures that a person does not appear twice in the index.
The Client Registration Workflow Chart

Visit Registration / Admission and Discharge
This application software is used for registering and ending the visit of a client. A visit is the period between arrival (registration) and departure (discharge) from the care facility. An inpatient visit is usually called an ‘admission’. A client is a person who has been registered in the Client Register/PMI and may be a new case or a follow up or repeat case. The Visit Registration application caters for the following functions:
- Confirmation of identity
- Registering an instance of service (the ‘visit’)
- Directing patient to the service/resource
- Facilitation of Charging and Billing
At the time of visit registration, it is important (for reasons of safety) to search for the patient in the Patient Registry using the the unique identification number (MRN) or other unique identification numbers (National ID/Passport) and ensuring that the appearance, age, gender, ethnic origin and photograph match with the patient.
A system generated unique visit number is given for each visit. This number indicates an instance of service and may act as the Financial Number for purposes of assigning charges.
During a visit, the patient may receive care through six (6) main service delivery systems/settings /locations i.e.
- Outpatient Care Services
- Emergency Services
- Inpatient Care Services
- Day Care Services
- Home Care Services
- Teleconsultation Services
At each visit, the patient receives part or all of the clinical care services. These include consultation, performance of diagnostic procedures (investigations), monitoring, treatment, supply of drugs / materials, nursing care and other clinical activities.
Services are provided by Clinical Service Units belonging to Clinical Departments. As a rule a visit to a department/unit providing direct patient care includes all direct care encounters and clinical support encounters. Therefore the patient is registered only once for a visit and need not be registered for each encounter. For in-patient services care may be provided by one or more clinical departments during the visit. Each encounter is recorded.
However, if an outpatient service is provided by another Clinical Service Unit of another Clinical Department it may be considered as another visit; even if it is on the same day. The patient is registered again for this visit and charged separately. This policy allows for a more convenient calculation of charges and collection of statistics.
There are occasions when, on a given date, the patient is provided only a part of the clinical care service, be it direct care or supportive service. This occasion (e.g. specimen collection, diagnostic imaging) may be considered as a visit despite having only a short encounter. So, the patient is registered for this. Whether charges are levied is a matter of policy. For example, the charge may be reduced or waived.
The type of Clinical service, Clinical department, room/resource and the primary provider providing the care are assigned based on information already available in Scheduling and Appointments or the Duty roster.
The design of the application must cater for the use of different meanings of terminology regarding locations, rooms, resources and care providers for Outpatient Care Services, Emergency Care Services, Day Care Services and Inpatient Care Services.
Charges are usually accrued for a visit i.e. based on charges levied for all services provided during the period. Charges are usually factored against certain criteria. The main factor is the charge category. Therefore, at the time visit registration the charge category of the client is determined by determinants such as the mode of payment, privilege for discount or exemption and other criteria. These data need to be documented.
Discharges
A patient is discharged once all care and certain administrative processes have been completed. This can be done manually or automatically. The discharge may be made manually by the care provider who performed the last process of the visit or a service (ward/clinic) manager. It would be helpful if he/she is able to view the task status on the task list and verify that all orders have been carried out.
For Outpatient Care Services and the Daycare Services, automatic discharge can be built in by applying rules such as:
- all orders/tasks have been completed
- at the end of the working hours
The second arrangement is acceptable because since if the clinic or unit is closed no further tasks can be performed anyway. However, it has the disadvantage of not ensuring that all planned tasks have been completed.
For Inpatient and Emergency Services, automatic discharge is not advisable since there is no limit to the working hours. The discharge criteria is not just the completion of planned tasks but also the fitness for discharge. Since the patient is domiciled at a fixed location a care provider (usually a nurse or nurse manager) can check whether the discharge criteria has been fulfilled and permit the discharge of the patient.
Visit Registration Workflow Chart

Maintenance of a Medical Record
From the legal standpoint, the institution where the care is given is responsible to maintain and make available an accurate record of the care given and events that occur during a visit. The institution is not responsible for keeping a record of what transpires beyond the visit. Hence the Medical Record consists of interrupted segments made up of record of events at visits attended during a care episode.
However, the events that occur in the intervening period between visits is usually documented during the latter visit as part of history taking for purposes of monitoring the illness and effects of therapy.
Use of Visit Registration System at Mortuary Services
The Mortuary can be considered as another location of service. The patient (who has died) is transferred to the Mortuary or discharged and readmitted to the mortuary (depending on the hospital policy). A unique visit number can be given for the visit to identify the dead body. Similarly, lists of dead patients located in the mortuary and tracking of processes should also be made available.
Bodies brought in from outside should not be registered in this system but in the Information system for the Forensic Services which is not within the scope of a Patient Care Information System.
CLIENT-RESOURCE MANAGEMENT SYSTEM
FUNCTIONS OF CLIENT-RESOURCE MANAGEMENT SYSTEM
The client-resource management function enables a service manager to assign a patient to the correct resource that matches their needs. These resources can be:
- Time period
- Service of a Care provider
- Physical site (Room/Bed/Couch)
- Machine (e.g. imaging machines, dialyser, treadmill, treatment machines e.g. ESWL)
A service consists of a set of tasks performed by appropriate care providers, using specified machines and approved methods in a conducive environment. A task can be performed only if the required resource is available. More than one resource may be required simultaneously e.g. a room, a machine and an operator. While some tasks can be performed on demand, most need to be planned (scheduled).
Allocation to a Service
A care episode refers to the sum of all visits for a particular health problem. It begins with the first visit and ends when care is discontinued. The number of visits per episode is by nature variable but may be intentionally fixed in a service package. A visit requires one or more identified physical resources such as room/bed within a clinic complex or ward. During the visit the patient may have one or more encounters with different care providers at the same or different room/bed. The duration of use of each resource is defined as time slots or sessions. The encounter itself may be timed to coincide with the period a machine is available for use.
The client-resource management function is performed using an application with three (3) functions i.e.
- Appointments and Scheduling
- Resource allocation, Staff-Job assignment, Creation of work-lists and Tracking of resource availability
- Patient Tracking
Differences in Approach between Service Delivery Settings
The service manager needs to coordinate the activities that a patient is involved in. It is expected that the above functions would be approached differently for the six (6) main service delivery systems /settings / outlets i.e.:
- Outpatient Care Services
- Emergency Services
- Inpatient Care Services
- Day Care Services
- Home care Services
- Teleconsultation Services
The policies, workflow, work processes and terminology regarding locations and resources are quite different for the four Service Delivery Systems even though they are actually just variants. As such, the applications software should be customized to suit each service delivery system.
For Emergency services, resource allocation depends on disease severity determined by triaging. For Day Care, patients may or may not be allocated to rooms, beds, couches or seats. Inpatients are transferred from location to location which can be temporary or permanent. For temporary locations, the original resource (e.g. bed) may need to be retained. These require a comprehensive bed management system. A home visit is considered as a service visit. It is scheduled and registered. Clinical notes are written and kept in the patient information database and so the EMR.
APPOINTMENTS AND SCHEDULING
The Appointments and Scheduling Application software is used for assigning a patient to the correct resource, at the right time and in the correct sequence. Persons eligible to use this application include care providers and the appointed administrative personnel (receptionists and clerks).
APPOINTMENTS AND SCHEDULING FOR OUTPATIENTS
The appointments and scheduling application software provides a solution for assigning a patient to the correct department/unit, facility, rooms/machine and care provider at the right date-time, for an appropriate duration and in the correct sequence. This appointment and placement is tentative. It is subject to modification and confirmation by both the patient and the unit concerned.
The application software provides a basic structure and layout of appointment books, pages (booklets) and slots for various departments, facilities, services and locations. It also provides information on the status of availability of the resources e.g. by indicating the rooms, beds or equipment that are empty or not in use.
Scheduling Application for Outpatients
Assignment of Patients to Resources

The software is equipped with tools for trained users to design new books according to needs based on the basic structure and layout. Each book have pages for sessions defined by the date and time period. Each page have time slots which can be categorized into different types based on user defined criteria such as availability, priority, ownership and privileges. Users are able to add, disable, delete and reserve slots. Each page of an appointment book displays the availability status of slots for each room denoting vacancy, booked / taken and non-availability, with the help of a colour scheme.
The application allows for the assignment of privileges for the use of slots to specific persons by care provider category or name. The software can be web-enabled to allow for integration with applications system of sister facilities or a centralized scheduling unit.
The Appointment Book, Booklet and Pages

Scheduling & Bed Management for Inpatients
The Inpatient Appointments and Scheduling (Bed Booking, Admit, Discharge and Transfer/ADT) application provides a solution for tentatively booking a patient to the correct department/unit, ward and bed at the right time and for an appropriate duration. Unlike in the outpatient setting, a visit often lasts for many days or weeks. The timing of encounters and consultations during the stay are flexible, such that there is no necessity to schedule them in time slots. Some tasks for example monitoring and nursing procedures are scheduled but the Order Entry application is used. The timing and frequency is determined when tasks are created.
The basic structure and layout of the bed-booking register for various departments, wards and beds is shown below:
The Scheduling Application for Inpatients
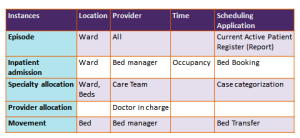
The software provides tools for trained users to design the bed-booking registers according to needs. Each page of the register should be for one day or session and it should be possible for the hospital to define the check-in and check-out time.
The application software enables the bed type to be classified based on user defined criteria such as charge rate, use (e.g. isolation, remand, intensive care), priority, ownership and privileges e.g. the allocation of the particular ward or bed to a particular department. Each page of the bed register displays the status of beds availability for each ward as vacant/available, booked and not available on a particular date and denotes the status by a colour scheme. A mechanism is available to search for available beds by bed type and location. The bed management application should enable the calculation of bed occupancy rate.
The application software allows for assignment of privileges for the booking and assignment of beds to a specific person, care provider category or name.
Appointments and Scheduling for Daycare Services
The specifications mirror that of the Outpatient service. The Daycare service is provided within the same day within a limited period which is divided into slots. In addition for patients undergoing surgery or procedures (e.g. endoscopy) when assigning the slot, the room where the procedure is to be performed must also be indicated. In this respect it is quite similar to the system for inpatients.
Appointments and Scheduling: for Common User Areas
Common user (shared across the hospital) facilities present some challenges mainly because resources can be limited and control of use of resources requires the intervention of a manager. Two approaches can be taken i.e.
- Sessions (time and location) are assigned beforehand to a particular care provider or care provider team.
- Slots are requested for and assigned by a service manager
A session (in this context) is a period containing several slots. In the first approach the entire session (whole day, morning or afternoon) is assigned to a care provider or a care-provider team (e.g. a unit). The care provider is then at liberty to slot in his/her cases within that session. If it is a team, there is a need for a coordinator to ensure that slots are fairly given to members of the team based on agreed rules. A good approach is to create a tentative list that is confirmed prior to the actual date.
In the second approach, care providers do not slot their patients directly but instead have to make a request to a manager / coordinator. He or she assigns the patient to a slot using her judgment based on agreed rules. This is especially necessary for services where resources are limited such as scheduling Emergency cases for surgery and anesthesia in the operation theatre and similarly for Imaging Examinations. To make the requests, the Order management system is used and a list of the requests appear in the manger’s in-box.
Allocation of Patients to Resources
It is important to differentiate physical locations with divisions/departments/units providing services. Often a location may be used by care providers from different specialties or units. Clinical Departments/Units are administrative divisions rather than physical sites.
The Appointments and Scheduling application enables the creation of a tentative list of patients arranged according to the room, time slot and the care provider. A confirmed list of patients in attendance is determined once they have undergone the Visit Registration. The Service Manager also need to know which resources are available and ready. He/she is then able to allocate patients to resources accordingly and validate the work-list (patient list) which can be integrated with the queue system. The application should allow the flexibility for the reassignment of patients to alternative clinical departments, clinics, rooms and care providers.
Staff job assignment (Rostering) should be part of the Client Resource Management System. It should enable all categories of staff to be allocated to work areas, rooms, wards, cubicles, beds, machines etc. according to dates and work shifts. Care providers need to sign in to confirm that they are available. The system should allow for constant updating of staff assignment. The application should enable the computation of the degree of efficiency of resource utilization.
Care Provider Assignment
There is a need to assign cases (patients) to a care provider. The clinical case manager who leads the care team is usually a doctor who is often referred to as the primary provider (doctor). Others in the team may be co-providers (other doctors and nurses) and providers of clinical support services that include:
- Nursing Services
- Rehabilitation Services
- Pharmacy services
- Anaesthetic Services
- Laboratory services
- Diagnostic Imaging services
- Others
The application should enable tasks to be assigned to individuals by name or by designation (e.g. person on duty) and work-lists created. It can also be used to determine client-provider relationship which in turn facilitates assignment of access privileges. This functionality within the Client-Resource Management Application is made available for all services / settings / locations, with some modifications.
Resource Allocation for Outpatients
The Resource-Allocation functionality provides information to the service / facility manager to optimize the use of resources. It is capable of creating and presenting a patient list of all patients of the clinic arranged according to the room, slot and the care provider they are assigned to, based on data from Appointments-Scheduling and the Visit Registration Application.
Allocation of a patient on follow up is simple in the sense that the case would have been assigned to a particular provider or provider team while previously warded or at the last visit. For new cases, the allocation is usually based on whether:
- case is referred to a particular care provider or care provider team
- the privilege or duty for providing the care (taking in) for that particular period (day or session) and for that type of case
The software should be designed to include tools for the allocation of a particular clinic or room to care providers of a particular department or named care provider.
The service / facility manager (e.g. sister in charge) should be able to reassign or reschedule patients to alternative clinical departments, clinics, rooms and care providers using the Appointments-Scheduling Application.
The resource allocation software confirms a patient-provider relationship between the patient and a designated care provider. This relationship is then linked to the application for assigning privileges of access and carrying out care processes.
Resource Allocation for Inpatients
For Inpatients, the Resource Allocation application provides the following functionality:
- Allocation of a particular patient to a named clinical department or service
- Placement of a patient to a ward and bed
- Acknowledgement of arrival of a patient at the ward and bed
- Assigning the patient to one or more care providers of various categories (doctor, nurse, therapists etc.)
- Present a patient list of all patients of the ward according to the room, date and care provider they are assigned to.
Resource Allocation for Daycare
The specifications should mirror that of the Inpatient service. Patients would have been assigned to beds /couches or procedure rooms. However, the work list for the day depends on attendance of patients and availability of resources. The application enables the manager to confirm the list, reassign cases to locations, providers and machines if necessary.
PATIENT TRACKING
The basic elements of clinical service are tasks such as consultations, procedures, observations, communications, education sessions and the supply of items. Incidences or events also happens to or are experienced by the patient. ‘Patient Tracking’ enables the user to be aware of the status of the administrative processes and patient location as well as attendances, admissions, transfers and discharges. The application also provides information on encounters and events. An encounter is the meeting of the patient with a care provider at a designated place and time for the provision of a service using various resources (facility or location).
The application software enables the acknowledgement for a visit and the automatic capture of the time by the clock as and when the patient has:
- been registered for the visit
- arrived at a location
- started an encounter
- completed the encounter
- been discharged (the visit ends)
This can be done using two mechanisms:
- White Board Functionality
- Search mechanism
White Board Functionality
White Board Functionality displays information in the form of tables/matrix on a computer screen. For in-patients and patients in Daycare, the “WHITE BOARD” can also be designed in accordance with the floor plans of wards. The “WHITE BOARD” is able to provide information consisting of the performance status, results of encounter, tasks and reminders. It would be of added value for the board to act as a graphic user interface (GUI) where selecting an item or icon within a cell of the matrix may initiate a software functionality including the entry of data.
This facility can enable the automatic calculation of time taken for patient to move from one location/encounter/process to another (time-motion data for quality control).
The application need to have a mechanism to search for and enquire about all the patients assigned to a care provider or to a clinical service/department/unit at any location. The white board can also be presented on a large screen with a read-only view.
The WHITE BOARD Showing Status of Patients at Endoscopy Suite

To enable this, reference or look-up tables need to be created for each patient in real-time by a query of the database.
Look up table of Order-Task Status Results for a Patient

Patient Lists or Work Lists
The tracking function should be capable of displaying the status of service provision e.g pending, started/in progress or completed as a work list. The beginning and completion of the encounter is recorded (as an acknowledgement rather than a registration) and tracked for use by the service manager (e.g. shown on a white-board) and for statistics.
Systematic use of the patient list or work-list ensures that:
- pending orders are attended to,
- tasks are performed,
- results are viewed
- documentation is completed
Locating Patients Using the Search Facility
The current location of the patient can be known by searching the database. This is dependent on users acknowledging the arrival of patients at various locations. Users can also determine what is happening to the patient by looking at the task status either in the work list or in the patients own order-task list. Such lists may be displayed on a white-board application and screen.
CHARGING-BILLING SYSTEM
Requirements of Charging and Billing Application Software
The Charging-Billing System is within the scope of the Hospital Information System. However the Patient Care System itself needs to be designed to transfer data regarding chargeable activities that has been performed or supplies provided. The actual assignment of the charge value, calculation of the bill is better served by an accounting application that includes also accounts receivable, payments made and credit balances.
Where feasible, the accounting application should be integrated with the proposed Hospital Information System and use the same hardware, network and system software. Additional hardware, such as bar code readers-scanners and printers or any other item, are necessary.
The payment system an entirely business function. The design is very much dependent on policies. In a government hospital for example, the collection of payments and issuance of receipts are subject to the Treasury instructions and would use a common billing and payment collection system made available by the Government (E-Gov). When necessary, links between the systems should be provided.
Charging Policy and Mechanisms
The application software should conform to the policies and mechanisms discussed below.
In a hospital, charges are incurred on the following:
- Hospitality services provided
- Tasks performed
- Items supplied
Various factors are used to determine the quantum of charges. These include:
- Service Delivery System/Setting/Outlet
- Financial Class/Charge category
Different rates are charged for the various service delivery systems i.e.:
- Outpatient Service
- Emergency Service
- Inpatient service
- Day Care Service
- Home Care Service
For each service, clients are further classified into classes or categories based on choice, privileges or by default. Assignment by choice occurs when the clients who pays ‘out of pocket’ select the grade of hospitality comforts (room type) that they can afford. The assignment based on privileges pertains mainly to eligibility or coverage set by payors (e.g. employers, health insurance). Evidence of eligibility is derived through proof of insurance cover or letter of guarantee of payment.
The application should allow for integration with third party systems such as the centralized government guarantee letter system (in Malaysia e-GL), health insurance schemes and others.
The items chargeable and rates depend on hospital policy. Charges for hospitality (bed) are often made only on inpatient care and day care services based on bed-type. For outpatient services, the policy may be to charge:
- a flat rate
- no charges at all
- charge according to type of room used
Each task performed or item supplied (drugs and consumables) must have a charge value. The quantum of the charge for the corresponding task or item is given in reference tables as determined by the hospital. Charges are incurred each time a task is performed or an item is supplied. It is up to the hospital to then charge the full amount or a discounted rate depending on the charge category or financial class that the patient belongs to. Charges can be waived for certain patients based on discretion or predefined criteria.
On the other hand, another approach is to charge a flat package rate for all services provided per visit, based on the type of visit or according to different types of packages for example defined by diagnostic related groups or even more general grouping such as specialty providing the service. Such an approach allows for flat pre-pay rate charges to be levied for all visits (as in government hospitals in Malaysia).
An instance of service for all service delivery systems in a hospital is the visit. The visit is defined by the time interval between registration and discharge. The total charge is calculated based on charges that accrue within that visit. The bill may have a list of items with the charge for each item which is then the total is summed (itemized billing). On the other hand, when a flat rate is charged only the total sum need to be shown.
Technical Methods of Calculation of Charges
The Charging-Billing System should be able to calculate charges based on factors according to policies set by the hospital.
It should be able to differentiate charges based on:
- Service Delivery System
- Financial Class/Charge category
It should enable the hospital to charge different rates for various service delivery systems i.e.:
- Outpatient Service
- Emergency Service
- Inpatient service
- Day Care Service
- Home care Service
- Teleconsultation service
The Charging-Billing System should enable the solution provider and users to build reference tables listing all chargeable items, the quantum of charges for each item and assign a charge code for each item.
The System should be able to:
- Facilitate the hospital to assign charges for a chargeable item either as a charge code or a fixed quantum
- Receive and accumulate charges for all chargeable items incurred by a patient based on data provided by the Patient Management application and the Order-Entry Result-Reporting application
- Calculate the total for each service instance (visit) by simple addition and also using various charging formula
- Produce a cumulative interim bill
- Produce a final bill
- Print bills on demand
Link between Patient Management & Charging-Billing Systems
The Charging-Billing System should acquire data on patient identity, registration, visits, encounters, discharge, service delivery system financial class and the payment method (out of pocket, insurance, paid by employer) from the Patient Management System (PMS).
Link between Charges and Order-Tasks
The Charging-Billing system has an interface with the Order-Entry Result-Reporting System (OERRS) and acquire data regarding all orders made and tasks performed.
For the purposes of creating an invoice, charges can be determined as soon as orders are made but for purposes of billing, charges are dropped only when the task is performed. The invoice is used if the hospital policy is for payment to be made up-front before a service is given.
The application software should determine the actual charge based on the charge code and make further calculations (discounts and mark-ups) based on policies.
Link between Charging-Billing & Bill Payment Collection
The Charging-Billing System should transfer information regarding clients, their financial class and charges incurred to the Bill Payment Collection System. Information regarding the payment method is also required but the data is obtained (directly or indirectly) from the Patient Management System (PMS).
Excellent work . I do appreciate your work to saving humanity
LikeLike
Dear Gideon.
Your appreciation will be my motivation although I am 73, sickly and immunocomromized.
Abdollah
LikeLike