First Published: Oct 6, 2021
Latest Revision: May 25, 2024
Please read the article on the Design of SOP/Care Plans before continuing with this article.
The Reference Care Plan/SOP is essentially built based on theoretical principles where conditions are assumed to be ideal. In creating Actual plans, an essential requirement is to understand clearly how the business of patient care is conducted in general and then within a specific organization, facility or setting, Therefore, every patient care organization or facility should develop SOP/Care Plans for its own care providers. The system o be used for implementation must anticipate what the care provider intends to do, show him /her the right direction and provide the necessary information. Next a mechanism must be established to help the care provider in put into practice these SOP/Care Plans as Actual plans. The reference plan is not converted into an actual plan as a new document, but pertinent parts are conceived as and when planning becomes necessary at various points of care. The care provider has to go back and forth between reading the reference plan and creating the actual plan This obviates reliance on memory. In this article I will try to explain the business of patient care as typically applied before trying to explore how actual plans can be constructed from reference plans in a separate article.
The Business of Patient Care
The SOP/Care plan functions as a guide as to what to do and how to do it. To make use of it, care providers must have a good understanding of the business of patient care especially with respect to how facilities, utilities, personnel and time are used optimally. There are many instances when it is necessary for the SOP/Care plan to be adapted before use; to cater for various conditions and factors that emerge as care is being delivered. Indeed, the business of patient care is a complex endeavor that needs a wider range of knowledge, skills, and experience.
Strict Adherence vs Use of Discretion
In most industries, to ensure that end products conform to specifications, the documented SOP must be strictly followed. Healthcare professionals, because of their knowledge and training in the management of diseases, feels competent at managing the multitude of health problems within their area of expertise. Persuading care providers to follow plans is a challenging task especially if the plans are rigid. Yet it is imperative that organizations and facilities must adopt business strategies that encourage adherence to SOP/Care plans.
In patient care, because of the complexity of the service, there is a necessity for clinicians to seek approaches they consider appropriate at their own discretion. This complexity is contributed by various factors including:
- minor variations in the disease or its presentation may necessitate significant changes in the plan
- peculiar situations may make it inadvisable or impossible to apply standard methods or modalities
- patients wish or preference
Patient care is delivered according to a universally accepted system that has been tried and tested over generations. The reference SOP/Care plans would have been developed with this system in mind. However, to put the plans into practice the care provider needs to have an understanding of the business of patient care. The word business here does not have commercial implications but refers to an organized activity aimed at a fruitful outcome. The use of SOP/Care plans must be in sync with the backdrop of the existing business model plus add value to it. The primary transformation that is hoped for is the realization of greater uniformity and standardization in the features and specifications of the service products. This aim should not detract from the necessity to consider the special needs of each individual patient.
Business Strategies
The organization or facility is responsible for instituting the following strategies:
- Getting care providers to understand the business of patient care.
- Finding the most suitable method of incorporating the SOP/Care Plan into the care of individual patients.
- Ensuring conformance / adherence to it with allowance for discretion in peculiar circumstances.
- Reviewing the success of implementation and improving on it.
Converting Phases of Care into More Quantifiable Units of Work
The Reference SOP/Care plan is constructed as if the entire clinical care is a contiguous series of activities. These activities (set of procedures and processes) are then grouped into phases (described earlier).
This division, while essential for understanding the content and flow of procedures, is not practical for the purpose of dividing the care episode into tangible service units. This is because phases:
- have variable content,
- take variable duration to complete,
- have no fixed start and end time,
- consists of procedures that may have to be performed at different locations
- do not allocate duties to specific persons or team/department/unit.
Therefore, the set of procedures for each phase must be converted into discrete units of service. This done by grouping procedures into modules defined by purpose, place and time, termed as sessions.
Sessions
Services are made tangible by offering them in workable batches or modules at appointed sessions. The term ‘session’ is a generic term used to indicate the occasion (event or happening) when there is interaction between the patient and the service delivery system.

Every session has two complementary purposes i.e.:
- for the patient: to receive a portion of care
- for the care providers: to conduct a set of activities.
A session is an apportioned time and space where a care-provider performs tasks as part of the service. Hence, it is defined and delimited by:
- purpose
- time slot,
- location,
- assignment to an identified worker or group of workers.
It is rare for a health problem to be resolved in a single session. Usually multiple sessions are necessary because:
- conducting procedures and obtaining their results require a variable time period
- a procedure can proceed to the next only if the required results or outcome has been obtained, some need to be repeated.
- some procedures are repeated at planned intervals
- certain transactions need to be performed at certain suitable locations
The purpose of the session is subsumed within the objective of the phase of care. The realization of this objective often requires more than one session. The time allocated must be sufficient to enable the proposed set of procedures to be done. The location must have the resources that match the requirements for conducting them. These may include proper environment, facilities, equipment and personnel. Usually, a resource may be used only by one patient at a time.
Visits and sessions are scheduled using an appointments book or a scheduling application. At each visit or session, the care provider must be aware of which phase of care of the patient is currently in. He or she should try to complete the procedures indicated for that phase of care or if unfinished defer it to another session. A thorough understanding of the relationships between ‘sessions’ and ‘phases’ is necessary.
Administrative and communicational processes must complement clinical care processes. The importance of the role that appointments, registration, and scheduling play in a care plan will be discussed in detail later.
Service Episode
The entire period during which a patient care service is delivered is termed as the Service or Care episode. An episode begins when a patient seeks help for a new health problem. The service ends, in most cases, with the resolution of the illness/problem or death of the patient. If the patient presents with a known problem for which he/she has been cared for in the institution, he/she will be managed within an existing episode.

Concept of Service Product
The services provided to the patient as a client of the institution is the service product. Depending on the nature of the health problem the service product will contain many service items (Visits, Sessions, Encounters and Events) which has to delivered through the use of appropriate SOP/Care Plans.
Planning for the Entire Care Episode
In a lifetime, a person may experience multiple illnesses, diseases or health problems. The entire period during which care is delivered for one of them is termed as the Care episode. It mirrors the disease episode. It begins at the time of first contact with a health care practitioner and ends when sessions are no longer required by virtue of the resolution of the illness or problem, being voluntarily stopped by the patient or by the death of the patient. A person may have many care episodes; with each episode being the time and effort allocated to a service product. For acute illnesses, the care episode ends when the disease resolved. For a chronic disease the duration is likely to be for a lifetime.
An episode remains active unless care has been discontinued. If a patient has multiple episodes, each episode is managed by a different team at a different visit or by the same team depending on the expertise required. Care is then delivered based on a SOP/Care Plans of each individual illness. Reference plans are generic. They give an overall and comprehensive view of the care to be given and the expected outcome for the entire care episode. The care provider constantly refers to them as the care progresses. He/she needs to be aware of the various alternative plans available because even if he/she starts with a particular plan for a certain problem, he/she may have to choose alternative plans later.
The actual plan is built based the needs that arise as care is given. As such it is tentative and becomes definite only when a definitive diagnosis is made and all the needs of the patient is known. If the patient has more than one illness the content of the plans has to be combined so that care is integrated and seamless.

It is important to differentiate care episodes for the purposes of:
- assignment and delimiting of the responsibilities of service delivery units e.g. specialty teams or departments
- allocation of funding, charges and remuneration
Shared Responsibilities and Continuity of Care
Patient care is delivered in tiers termed as primary, secondary and tertiary services at suitably equipped service delivery facilities.

The primary care facility is where the patient has his or her first contact with the healthcare service. At this tier, care is provided by general practitioners, family doctors or emergency care professionals. At subsequent tiers, the responsibility is taken up by specialty units.
Care episodes are assigned to appropriate facilities and units based on specificity, complexity of the health problem and the sophistication required for its care. Patients move across these tiers as care progresses. At each facility the care is shared between care providers with different knowledge and skill set. Work lists are used to assign tasks.
Therefore, at the earliest stage it is best that a general practitioner sorts out the disease type and direct the patient to the next facility. A referral would ensure that information already gathered about the patient and the treatment already given is passed on. It is not appropriate for the patient to seek care directly from a tertiary facility. Even after obtaining care at a tertiary facility, the patient may be better off getting the rest of the care such as rehabilitation and follow up at a secondary or primary care facility. In this way, the continuity of care is maintained while enabling patients to be managed at the facility that is most appropriate for their needs i.e. convenient, accessible and affordable.
Use of SOP/Care Plans for the Allocation of Funds, Charges and Remuneration
Since SOP/Care Plans promote uniformity and standardization, they provide legitimate basis for costing and charging. Organizations that provide funding (governments, insurance companies) can budget or reimburse based on activities indicated for each care episode or parts of it. Patient care facilities should also charge for services on the same basis. SOP/Care Plans provide the rationale for allocation of funds based on case-mix and beyond that funding based on capitation.
The use of care plans can obviate superfluous insurance claims, provide a fair mechanism for the distribution of funds and encourage prudence in the use of resources.
Dividing the Care Episode into Sessions
From the perspective of service delivery, even though the SOP/Care Plans are made on the basis of phases, their actual implementation happens at sessions i.e. instances where and when the patient interacts with the service delivery facility. Dividing the care episode into sessions with intervals in between makes the service more practical and quantifiable.
- Care Episode
- Sessions
Sessions are used in a generic sense as well as a specific service instance. They would be broken further into various types. Each session type has the following characteristics:
- defined purpose (why)
- defined content (what)
- performed at an allocated time (when)
- has an anticipated duration (for how long)
- performed at a known location, facility or setting equipped with appropriate resources and a conducive environment (where)
- performed by a care provider or team of providers (assigned to whom)
The division of sessions into various types i as depicted below:

Time slots are durations in minutes or hours making up a session. A visit may take a few minutes or days to complete depending on the tsks to be done. The visit is then divided into the required number of sessions. Often, a session is a meeting (encounter) with one particular care provider (doctor, nurse, therapist etc.) and therefore it can be equivalent to an encounter. However, there are instances where more than one care provider is involved simultaneously in the care of the patient, either performing the same or different tasks. So, there may be more than one encounter per session.
Events are things that happen during a session. It can be a planned task / procedure or an unexpected happening that requires a corresponding response.
Anticipating Future Actions
Planning is about anticipating future progress and actions. Procedures belonging to a phase are carried out one after the other for as long as the time slot or other constraints allows. Otherwise, what remains are pursued at future sessions.
For each patient, how the intervals between sessions are fixed depends on
- the urgency to move from one phase to the next.
- whether results of procedures (investigative or therapeutic) are ready
- the anticipated speed of progress of the illness
- the predictability of the response to care
- the need for iteration of procedures
- the need to wait for the availability of resources
It is important to base the duration of intervals on the behavior of the disease (its natural history), and the response to the care given.
Matching Clinical Care Settings with Nature of Illness
In acute cases, the condition of the patient changes quickly. Therefore, there is a need to move quickly from the activities aimed at determining the definite diagnosis to the activities of implementing definitive care. Procedures must be performed quickly and the results reviewed as soon as they are available. Therapy must then be started immediately. Hence, patients are seen very frequently; as often as daily or more frequently for purposes of observation, monitoring and review. This can only happen in an inpatient or emergency setting.
In a less urgent case, intervals between visits can be longer. Most cases can be managed as outpatients or at daycare sessions. Observations and monitoring can be done on arrival or by the patient at home. Certain processes such as tests, dressings, exercises, education and so on can be done as separate sessions rather than during consultations.
Achieving the Objectives of Each Phase
Usually, the objectives of each phase are not achieved by one run of procedures. In most cases, they are met only through a series of purposeful cycles, repetitions or iterations. Repetitions take time and often cannot be completed in one sitting, hence requiring additional sessions.
Resources in patient care are always scarce. A session can only be conducted if resources are available i.e the time and place is free and not otherwise already in use. Emergency cases take precedence to the extent that resources must be freed to to accommodate them. For chronic cases the care provider may exercise a bit more discretion.
The final objective of an episode depends on achieving the objectives of each phase. Therefore, evaluation of conformance to the care plan and the achievement of objectives must be done continually or at intervals as part of process control and audit.
Schedules and Appointments
Services must be provided in an orderly and predictable manner. This is achieved through through ‘scheduling’ i.e. the assignment of services according to fixed time slots, locations and care providers. Patients are assured of access to care by giving them appointments. Sessions are assigned as time slots. Turns to receive service items are allotted using a queue system.
Converting phases into sessions assures the patient that he/she will receive care in a predictable manner. However, healthcare is not as predictable as in industrial services. The time taken to complete various sessions are not very certain because it depends on many variables. The progress of the workflow for a particular patient varies depending on how his/her disease, illness or health problem behaves according to its natural history and its response to treatment. For the purposes of time management, when a session starts and ends depend on the variable duration taken for:
- the patient’s previous session,
- the session of the the previous patient.
Hence, times and periods allocated to sessions cannot be fixed firmly but simply estimated. Being too strict may push the care provider to rush through tasks. Being too lax will lead to time wastage. This uncertainty is mitigated somewhat by the use of queue systems.
Matching Workflow with Schedules
The process of scheduling is not a matter of fixing a session to an empty time slot. It must be taken seriously. Proper scheduling depends on the matching of several factors that include:
- The Visit type to the Case type
- Duration of Sessions to tasks / procedures being planned
- The Service delivery facility (room choice) to tasks / procedures being planned
- Matching the interval between visits with the natural progression of the disease and the response to treatment
- Ideal interval and date
- Acceptable approximate date and time
- Preference of patient and convenience
However, in healthcare the resources available (time, space, persons) are scarce and finite. A such to match schedules with the Care Plan / SOP is challenging. It is imperative that scheduling is based on a request where data regarding the needs of the patient s matched with the availability of resources.
Matching Schedules with Needs
efficiency, preference. Procedure and Continuity of Care
- by request
- ad hoc
inpatient what can be done during the day vs at night, early in the day, maximize the inpatient stay, do the most possible. Anticipation and planning. Normal pregnancy as an example.
DIVISION OF SESSIONS INTO VISITS
The care episode is divided into a hierarchy of sessions made up of all instances when a patient seeks services from a healthcare facility. First of all, it is broken down into service-delivery sessions called ‘visits’ with intervals in between. The visit itself is divided further into smaller time periods and service packages. The topmost level of the hierarchy is as shown below:
- Care Episode 1
- Sessions
- Visit 1
- Visit 2
- Visit n
- Last visit
- Sessions
- Care Episode 2
The number of visits for each phase depends on the number of visits required to accomplish its objective. This cannot be determined with certainty.

DEFINITION OF A VISIT
A visit is an instance when the patient comes to the health care facility to receive care. There is an interaction between him/her with the patient care facility and in most instances he/she has to be physically present. The visit is a session that occurs at a specified location and is bounded by time. It contains a set of services. It is formalized by the process of registration and ends with that of discharge. However, the term visit is also applied to instances when the patient is visited by the care provider (as in home care) and also when the interaction is virtual rather than physical e.g. in teleconsultation.
Relationship between Visits and Phase
The care provider plans events according to the workflow of the relevant phase of care described in the Reference SOP/Care Plan. So, even as the service is broken up into visits, he or she has to be acutely aware which stage of the workflow the patient is currently involved in and not lose sight of the overall plan. In many instances, phases would not coincide with visits. It is necessary that objectives of each phase be taken as the driver that moves forward the flow of procedures.
Purpose Of Visits
Visits are the sessions during which the care providers executes the activities of the phases of care delineated in the reference SOP/Care plans. For most diseases, it is not possible to group procedures discretely to match accurately with visits in the Reference plan. The care provider has to decide in the Actual plan when a visit should happen, where and what procedures would be performed in it.
Case Types
A visit is necessary for one of these purposes:
- Enrolling and starting services for a new case
- Continuation of care of a follow up case
At the beginning of a visit the care provider has to determine the purpose or reason for the visit. He/she is then faced with the question of what to do for the visit.
This depends very much on whether the visit is the initial visit or a follow up visit. The primary purpose of the first visit is to gather information for the purposes of making the diagnosis. The actions to be taken for subsequent phases of care are performed if the opportunity is available at that visit. Otherwise, those are pursued at future visits.
The activities to be performed at a follow up visit can be planned because information about the patient is already available from the previous visit. The diagnosis may have been worked out and a plan has been initiated. In this way, at the beginning of a follow up visit, the attending care provider knows the purpose of the visit and the tasks to be done. However, he/she may have to modify it based on any new information.
The period required to complete each phase is variable. It can span a duration of mere minutes or can be across many visits. The sequence and content of visits do not coincide necessarily with the anticipated change-over from one phase to the next. For each case type or sub-type, what can be accomplished during a visit is variable depending on many factors. The frequency of and intervals between visits is based mainly on the natural history of the disease and the patient’s expected response to treatment. When developing the Reference plan, the number of visits required to complete a phase can be anticipated through experience or derived from lessons learnt from analysis of historical data. The content of the service for some diseases, illnesses and health problems can be predictable. As such, the number and frequency of visits can be intentionally fixed and the service offered as a package.
However, in most cases the time taken to conduct procedures and to obtain results are very variable. Therefore, case managers or the primary provider decides on when and how often visits are to be made are at their own discretion when devising the actual plan.
In general, visit types are divided into visit types as categorized below:
- INITIAL VISIT OF A NEW CASE
- Planned Initial Visit of a New Case
- Unplanned Initial Visit of a New case
- FOLLOW-UP VISITS
- Planned Visits of Follow Up Cases
- Unplanned Visits of Follow Up Cases
INITIAL VISIT OF A NEW CASE
Patients may make choose to visit a healthcare facility in two ways:
- by prior appointment (scheduled)
- unplanned (walk in)
The visit formally begins when the patient is registered. The patient then becomes a client or in common parlance a ‘case’. For a new case, he/she has to be enrolled first as a client and then registered as a patient for the visit.
At the end of a visit, activities for the next visit must be planned. The proposal for what is to be done at that visit must be thought out and documented as part of the follow up plan.
Planned Initial Visit of a New Case
A planned visit for a new case merely means that the patient has made prior arrangement with the facility. For non-urgent patients (elective cases), visits are scheduled by creating appointment slots in time-tables of appointment books or a computerized scheduling application.
The scheduling system can be used to:
- allocate a time slot,
- determine an appropriate service location (facility, specialty department or unit),
- assign the case to a care provider.
Sorting Out New Cases
It is possible and beneficial to identify different categories of new cases. These could be:
- Cases with a known problem identified at other units within the same facility
- Cases referred from other facilities
- Patients who volunteered information at the time of making appointments
When requesting for an appointment, the patient may volunteer his or her reason for visit. This would enable the person giving out the appointment to be aware of the relative urgency.
On the patient’s arrival some information may be available from the previous care provider in the form of :
- referral letter,
- email,
- phone call
- message.
The ‘reason for visit’ may be established when the patient arrives. He/she can be assigned to an appropriate service unit, be given a queue number and served in turn. A rough plan based on the reason for visit can be initiated. It may or may not coincide with what is actually required. Proper plans can be conceived only after a triage process where some clinical data has been gathered by a person with clinical training and a preliminary diagnosis (symptom complex, clinical syndrome, diagnostic related group) is made.
Unplanned Visits of New Cases
Unplanned new cases are those where no prior arrangement is made. They are also called walk-in cases. New cases with urgent problems can seek services at emergency units without prior appointment. Some facilities e.g. general practitioner clinics may offer services for elective cases to walk-in patients. Such cases need to undergo the process of triage. This is a standard procedure at emergency departments but is also helpful for part of the initial service for outpatient care. The triage process is done by clinically trained staff at the reception or a suitable area.
Planning of Visits For Follow Up Cases
Follow up cases are those who had prior visit(s) at the facility for the same problem. Follow up visits are usually planned but patients may also arrive without prior appointment.
For the majority of instances, visits are planned and scheduled as a part of the actual plan at the previous visit. Follow up visits are necessary for continuity of care and this is determined at the end of each visit.
Moving on Through the Phases
Follow up visits are necessary to complete the remainder of the phases of care and thus ensure continuity. Many factors are taken into consideration when determining the frequency and regularity of visits. Occasionally, one follow up visit is sufficient but for the majority of cases, multiple visits are necessary.
At the start of a follow up visit, the decision to move on according to plan is made only after the patient has been reviewed to determine whether his or her status allows it. This is especially true if it is uncertain if the objectives of a phase of care is achieved. It may then be necessary to reiterate some procedures until sufficient information is available. This is even so in cases where the disease inevitably progresses such that the care provider may have to make decisions without precise information. For example, in ante-natal care where plans are made for phases coinciding with trimesters of pregnancy. While the pregnancy inevitably progresses making it necessary to perform certain interventions. While doing so, processes or interventions that have not been successfully completed are continued or repeated as indicated in the care plan and any missing information is obtained.
The above example illustrates the reality that despite the use of SOP/Care Plans, some decisions and actions are at the discretion of the care provider.
Unplanned Follow-Up Visits
Follow up cases requiring urgent attention (due to deterioration or development of complications) may avail themselves to services as and when they require them (unplanned). Such patients also come into the category of walk-in cases and the facility must be ready to receive them. On arrival, they are triaged, listed into groups according to priority, placed on a queue and served according to their turns.
Frequency and Intervals Of Follow Up Visits
The interval between one visit or encounter to the next is dependent on two factors:
- the expected behavior of the disease according to its natural history,
- the expected duration for the treatment or intervention to take effect.
The visit interval can be roughly indicated in the care plan based on the natural history of the disease and its response to treatment. Yet, in most instances it is estimated at the discretion of the care provider. The actual fixed date is very dependent on the availability of resources. Often this duty is delegated to administrative staff (clerks or receptionists) who would then use the appointments book or scheduling application for this purpose. Intervals between encounters or tasks are managed using a queue system. This delegation of duty must be based on close understanding between clinical and administrative staff.
Sequencing within the queue system is usually on a first come first served basis but due consideration must be given for children and the aged.
How procedures within a care-plan are sequenced may vary depending on circumstances. As such, the procedures may be performed at the beginning of a visit or in the middle of a visit. A phase ends when the set of procedures are completed and the defined objective is met. If a phase cannot be completed at a visit, the patient goes home and the procedures are continued at the next visit. Hence, phases may start or end at different visits. At a visit the care provider must be aware the phase that the patient is at.
There are situations where the transition in the flow of the care plan is predictable such that a change-over of the phases can be initiated as and when the visit takes place. Good examples are the care plan for the care of a patient with normal pregnancy and a patient undergoing knee replacement surgery.
Legal and Operational Implications Of Visits
There are legal implications applicable to both the patient as well as the care provider when a patient seeks care or is given care. The first visit is the beginning of a care episode. It always begin with the phase of formulation of diagnosis and early treatment. Subsequent visits are continuation of this phase or progression to the next. It is assumed that the patient comes willingly and will abide by the rules set by the facility. Hence, for many processes it is assumed that tacit approval from the patient has been received. However for certain procedures, it is necessary for the patient to provide either verbal or written consent. The care provider as an organization and individually is obliged by law to exercise care when providing services. These obligations are often written and displayed as the Patient Charter.
The above reasons make it necessary for patients to be inducted into care through the formalized process of registration and release from it with the process of discharge.
It is also a legal requirement for care providers to keep a record of what transpires during the visit as the medical record. A compilation of records of individual visits make up the medical record of the patient. The obligation to exercise care and to record events (planned and unplanned) is applicable to all visits except for self-care where the onus is on the care provider to provide guidance and the patient to follow it. Hence, the medical record is a compilation of records made at visits.

Location (Setting) of Visits and Differences in Visit Types
Services by necessity must be delivered at specific locations. Each location is a service delivery unit with specific settings i.e. the facility design (layout), environment, and the resources made available. Hence, visits can be divided into types based on locations or settings that include:
- Outpatient visit
- Emergency visit
- Inpatient visit
- Day Care visit
- Home Care visit
- Teleconsultation visit
- Self-care
Each visit must be matched with an appropriate setting. Hence during the care episode, a case may be managed at some or all these visit types.
Choosing the Appropriate Setting For Various Visits
The type of service delivery setting for each visit must be planned. Only in some instances, the most appropriate service delivery setting for a particular visit can can be predicted and decided in advance in the reference SOP/Care Plan. Some illnesses can be managed completely at an outpatient setting, others need to be cared for at a day care units as part of their care. Yet, most acute cases must be managed at inpatient wards or the emergency uniut at least at the beginning of the care process. However for many types of diseases, the decision has to be made when formulating the Actual plan as the care progresses.
The service delivery setting chosen should be make it feasible to perform the actions planned in the SOP/Care Plans. Certain resources (environment, equipment or personnel) available in an inpatient or day care setting may not be available at an outpatient clinic.
The Emergency Setting
The Emergency setting is designed to provide care for cases requiring urgent attention, close observation, resuscitation and stabilization. It receives walk in patients and provides services on a 24 hour basis throughout the year. Patients are triaged and categorized based on urgency and severity. The layout, equipment and staffing is designed to cater for the needs of each category.
Patients with minor illness may receive sufficient care at the Emergency unit to enable them to be discharged with or without follow up visits at regular clinics. However, for most patients, the Emergency visit occurs prior to further care at the in-patient setting.
The Ambulatory Setting
When the progress of the disease is gradual and the effects of treatment take time to manifest, the case is better managed as an outpatient.
An ambulatory visit is restricted to the maximum of one work day. There is a limit to the number of tasks that can be completed. This means that, blocks of procedures have to be planned for each visit in a more discreet manner.
For cases managed in the ambulatory setting (outpatient or daycare), the patient goes home and comes again for another visit to the facility. At a follow up visit the patient’s progress is reviewed and the decision to move through the phases is usually made then. Between visits, care providers will have to depend on patients to practice self-care i.e. monitor their own symptoms, signs and physiological or biochemical parameters by performing simple tests.
In between, the patient may avail himself/herself to teleconsultation, be given home-care through home visits by care providers or manage on their own (self-care).
Day care is a setting that is a cross between inpatient and outpatient settings. It allows more complex investigation and treatment procedures to be done. The patient can also be observed for a longer period. It is suitable for care taking a duration of more than a few hours but less than a day.
The Inpatient Setting
In visits at an inpatient setting, the patient stays in the facility allowing the care provider to observe and monitor the patient frequently. As such, there is opportunity to review the care plan for the case as often as daily or more frequently and decide on the readiness to advance through the phases. Also, certain resources are available only in the inpatient setting. Hence, it is suitable for the care of either acute illness or the initial care of chronic illness. The inpatient visit allows the care activities to be repeated within the same visit. Patients rests in between activities and are provided with lodging, food, beverages plus other necessities.
Differences In The Care Of Acute vs Chronic Illness
In acute illness the disease progresses at a rapid pace. Hence, tasks are also performed rapidly at short intervals or continuously. This means that the appropriate service delivery setting for acute illness at the immediate phase is either the Emergency Unit or the Inpatient facility including the Intensive Care Unit and the Labor room. Efforts are directed towards symptom relief, resuscitation, stabilization and support (physiological, psychological, social and spiritual).
The care of a patient with chronic illness begins with the initial contact with a health care provider. The disease process itself may be at an early or later stage of the natural history of the disease, depending on whether the patient seeks treatment early or late. At the earlier phase, the main objective is to determine the diagnosis as accurately and comprehensively as possible.
The care of a patient with chronic illness can be carried out a slower pace. Chronic diseases are suitably managed as outpatients. The exception is at the start of care of certain diseases where a short stay in an inpatient setting is required for the purpose of close monitoring, stabilization or optimization of therapeutic regimens. Care of outpatients occurs at visits spaced at intervals. The appropriate interval between visits is determined by:
- the expected speed of progress of the illness,
- the time when of results of tests will be ready,
- how fast the effect of treatment will become apparent.
The interval between visits gives time for the care provider to obtain a diagnosis with a high degree of certainty and the choice of the most appropriate definitive care plan. Involvement of the patient in care of his/her own self at home is essential. For incapacitated patients, those looking after them (relative or friends or hired aids) will take that role. The same is true for parents in the care of their children.
When the diagnosis is certain, definitive treatment is initiated. Even so, often optimization of the therapeutic regimen cannot be accomplished in one sitting. Unless it is the treatment of an emergency case, the effects of treatment will take time to manifest. So, treatment is followed by monitoring of the patient which includes checking on the progress of the illness as well as assessing of the benefits of treatment and the side effects. Rehabilitation would be added to the plan, in earnest. Progress review is done regularly to determine the effectiveness of the therapy. Failure due to non-compliance to the plan by care providers and patients need to be excluded. Once an optimal regime is established, it should be continued until desired outcomes are achieved.
If the success of the plan itself comes into question, there is a need to review the reliability of the diagnosis and the appropriateness in the choice of the plan or the way it is customized.
Further Division of Visits Into Sessions for Performing Procedures and Responding to Unexpected Events
Having divided the care episode into visits, the next step is to plan what happens during the visit. For this purpose, the visit is further broken down into smaller sessions where actions take place. During the visit two types of actions are often necessary:
- procedures planned in advance
- procedures in response to unexpected happening.
The session itself can be equivalent to a procedure. In the reference SOP/Care Plan the activities planned consist of procedures grouped together in blocks according phases of patient care (discussed earlier). Besides these, there are instances when unexpected happenings occur and procedures are performed in response to them.
The hierarchy of sessions following this division is as shown below:
- Care Episode
- Sessions
- Visit 1
- procedures planned in advance
- procedures in response to unexpected happening
- Visit 2
- Visit 1
- Sessions
The patient care workflow are made up of procedures arranged in sequential phases. A phase is defined by its objective. The care provider may vary the sequence of procedures to adapt to circumstances for the sake of efficiency, convenience and in response to peculiar needs; as long as the objectives of the phase of care are met. As such, the procedures may be performed at the beginning of a visit or in the middle of a visit. However, all procedures necessary to achieve the defined objective of a phase must be completed. In the outpatient setting, if the procedures within a phase cannot be completed at a visit, the patient goes home and the procedures are continued at the next visit. In an inpatient setting, the patient is retained until the procedures are completed or is discharged and the procures are continued at a follow up visit. Hence, phases may start or end at different visits but the care provider must ensure that all necessary procedures of each phase are performed and the objectives are met.
Planned Procedures
Planned procedures are those expected to occur as part of the service. The word transaction may be used instead but it has a more commercial tone. As noted earlier, it must be emphasized that visits and therefore procedures within them do not coincide necessarily with phases. However, the accomplishment of the objectives of various phases are the drivers of the flow of events. The care provider plans procedures according to the workflow of the relevant phase of care described in the Reference SOP/Care Plan (and will be discussed in detail later). Hence, he/she has to be aware, at all times, which stage of the workflow he or she and the patient is currently involved in.
The use of SOP/Care plans will enable almost all procedures of patient care to be planned. During these events one or more tasks may be performed. Each task is done:
- for a purpose,
- at a scheduled time,
- at a facility or setting with suitable equipment or resources and a conducive environment.
- by an assigned care provider or a team of care providers.
How procedures within a care-plan are sequenced may vary depending on circumstances. As such, the procedures may be performed at the beginning of a visit or in the middle of a visit. Procedures are considered completed when the desired outcome is achieved or the result obtained. In complex cases, the set of procedures planned for a phase may be completed only after a few visits. In simpler cases, completion of events of one phase or more can be accomplished in one visit.
A phase ends when the set of procedures are completed and the defined objective is met. If a phase cannot be completed at a visit, the patient goes home and the procedures are continued at the next visit. Hence, phases may start or end at different visits. At the beginning of every visit, the care provider must be aware the phase that the patient is at.
Purpose of Procedures at a Visit
The procedures to be performed at a visit is dependent on what is planned for the current phase of care. The phases of care are fairly standard but because clinical care is iterative in nature, any, some or all of the following procedures (administrative and clinical) may be performed at a visit. The phases are as listed below. The procedures contained in each of them will be discussed seperately.
- Care Episode
- Sessions
- Visit 1
- Registration
- Triage
- Review of available information
- Visit 1
- Collection of information through interview, examination, tests and investigations
- Formulation or review of diagnosis
- Planning of care
- Observations and monitoring
- Response to incidents or untoward events
- Progress review
- Review of plan
- Decision on Continuation or Discontinuation of care
- Discharge
- Visit 2
- Sessions
Review of Available Information
At the start of a visit, it is important for the care provider to review currently available information. For a new case these may take the form of referral letters or shared lifetime health records. For cases already receiving care, entries in medical records at previous sessions and the medical record summary should be read. In a computerized information system, the information is provided as views and reports.
Collection of New Information
Collection of new clinical data (symptoms and signs) are always carried out at every visit. This procedure is made up of interview of the patient, physical examination and simple tests. For a new case, The objective id to acquire sufficient information to make a diagnosis and identify the patient’s health status. For follow up cases, the changes in the status of the previously known problems need to be assessed through monitoring and observation. New problems that emerge should be identified.
Review of Diagnosis
The diagnosis is reconsidered at every visit and updated in the medical record or the information system when a change is made by the care provider.
The performance of tests and retrieval of results may be spread over different visits. Treatment too may be ordered at one visit but carried out at another visit often at a different setting. The immediate effects of treatment should be detected or if not immediately obvious, are appraised at a later visit.
There are instances when a care provider would attend to a case more that once during the visit by repeating a procedure, adding an extra session, procedure or to review results when they are ready. In other instances, when responses are slow to manifest or results take time to be ready, the patient goes home and comes again for another visit to the facility.
Procedures Related to Unplanned Events
Besides planned events, there are instances when unexpected happenings occur. These include:
- incidents,
- side effects or complications of treatment,
- unwanted developments,
- mistakes.
When these events happen two types of actions must be performed:
- acknowledgment or notification of the event,
- response to it.
The event is observed, noted and recorded. If the event has not been observed by a care provider, a history is taken from the patient or by-standers. Actions are taken to counteract the effects of the unplanned happening. Documentation of the incident and the response to it can be considered as one event or separately. Besides recording in the medical record, certain events require mandatory notification (incident reports).
Anticipating Events and Readiness to Respond
Some unwanted effects are not necessarily random events but are known to happen and can be anticipated. In the preparation of the Reference SOP/Care plan, actions in response to them are prepared in advance and documented. However, care providers must be prepared to respond to any type of unexpected development. Examples include:
- electrolyte imbalance
- acute respiratory failure
- acute renal failure
- cardiac arrest
- anaphylaxis
- falls and injuries
- adverse drug reactions
- anxiety an depression
Use of Work Instructions
These type of occurrences may happen during the management of any disease. Instead of including their management in the SOP/Care plan the procedures are written in detail as Work instructions which would be used repeatedly through out the facility. The work instructions should be available to all care providers who should also be trained rigorously on how to carry them out.
Types of Procedures
The term procedure is used in industries to refer to units of work comprised of a set of processes. The term ‘task’ is commonly used in healthcare. The term procedure is preferred in this discussion but the term task will be used where appropriate.There are many types of procedures, categorized according to various criteria i.e.,
- the method used,
- the persons involved in their performance,
- sequential or concurrent,
- the setting where they are carried out.
Types of Procedures Based on the Method Used
Care providers used various methods when accomplishing procedures. These include:
- technical (with or without the use of machines),
- cognitive (reading, thinking, interpreting, making decisions),
- communications (talking, listening, expressing and understanding body language) or
- documentation (writing, data entry)
Often the methods are used in combination.
Types of Procedures Based on the Involvement of Persons in Their Performance
The patient care service is accomplished through the involvement of different groups of healthcare professionals. There are those who deal directly with patients while others contribute in a less direct manner. Events (procedures) may be conducted in the following ways:
- face to face interaction between the patient and care providers (encounters),
- performance of actions without the necessity of the presence of the patient (non-encounter events, events sans-
encounter), - actions performed on specimens taken from the patient (tests on specimens or samples).
Division into these types is important with respect to allocation of responsibilities, sharing of information, and reimbursement.
Procedures Performed at Encounters With Care Providers
Many tasks can be performed only during face to face meetings between the patient and the care provider. The term ‘encounter’ is used for such an event. Most clinical procedures are performed at encounters. The actions include those that involve:
- speaking with and listening to the patient,
- physical examination and observation,
- performance of measurements and tests on the patient
- procedures or interventions
Direct care is usually given by clinicians, a term often reserved for doctors where the sessions are termed as ‘consultations’. However, many other care providers provide care directly to patients, use the clinical care process model and therefore have encounters with patients. Therefore, the following professionals should also be regarded as clinicians:
- Nurses
- Optometrists
- Audiologists
- Therapists (physical, speech, occupational)
- Clinical psychologists, counselors
Although they often provide clinical support, there are instances when they would be working independently as practitioners.
Care providers performing clinical support functions also perform procedures at encounters i.e. in direct contact with the patient. Such providers include:
- Radiologists,
- Radiographers,
- Echo-cardiogram technicians
- Endoscopists,
- Phlebotomists
Some procedures that they perform are at encounters with patients.
Procedures Not Involving an Encounter with a Care Provider
A procedure need not necessarily be carried out during face to face encounter with patients, Care providers may perform actions on their own without the presence of patients (procedures sans encounter). Such actions include:
- thinking (cognitive) actions e.g :
- review of information and deriving conclusions,
- the formulation of diagnosis and
- selection or modification of plans
- any form of decision making,
- preparatory activities performed before procedures,
- actions performed on or by machines.
Often, these actions are not considered as procedures that are part of the SOP/Care Plan. On the contrary, they should be planned, ordered, and recorded in the medical record, unless they are so routine that they can be assumed to be done.
Procedures that are part of information management can be performed, at any time during the visit, without the patient being present. Normally, the first action that a provider does at the beginning of a clinical session is to review the existing data regarding the patient, These can be reviewing the case summary, the monitoring chart, results of investigations done previously (pathological or radiology tests) or notes made by other care providers. At the end or in the middle of the session, he/she may formulate and document data regarding the diagnosis, assessments and opinions. He/she may communicate with other care providers directly, by phone or by forwarding referrals or replying to them. In a new case, before attending to the patient, the care provider can read the referral letter and results of tests already performed that came to him/her with the patient or submitted by other means.
Preparatory activities, like the admixture of medication and setting up of equipment or instruments before procedures, are also done without the patient being present. It also includes communication between team members. Some of these are routine and it is not necessary to be included in both the reference and the actual plan or recorded in the medical record.
All these procedures take the care provider’s time and effort. They must be considered when organizing patient care activities.
Tests On Specimens or Samples
Tests are events that are often performed on the patient (e.g. taking images, EKGs, EEGs, Audiometry, Optometry etc.) during encounters.
However, there are tests performed on samples from the patient rather than the patient him/herself. A big advantage is that such procedures can happen concurrently and at different locations.
Intervals between Procedures (Wait Time)
In healthcare, very often results or outcome of a procedure is not immediately available. Hence for some procedures, intervals during which there is inactivity and waiting are necessary before moving on to the next. Intervals between procedures are managed using the appointment book or a scheduling application software coupled with a queue system.
The intervals between procedures are determined by the:
- availability of resources (free slots)
- batch management
- process time
- turnover interval
Sequencing and Spacing of Procedures
Sets of procedures are performed to achieve a purpose. Planning of procedures is only possible if the sequence of steps can be anticipated in advance. Otherwise, the care provider has to make judgments on the necessity, priority and frequency of procedures. This will come with practice and experience.
At a visit, not all of the procedures will be performed strictly according to the flow of the clinical care process or the usual sequence. Review of existing data and collection of new clinical data (symptoms and signs) are always carried out. Review of previous values of monitoring parameters and repeat measurement of them almost always occur at visits. The status of the previously known problems need to be assessed and new problems that emerges are identified. The diagnosis is continually reviewed and based on the possibility of a change, further investigations are planned. The investigations are planned and ordered at a visit but may be carried out at other visits. The performance of tests and retrieval of results may be spread over different visits. The intensity of monitoring is reviewed depending on the patient’s condition. Treatment may be ordered at one visit, carried out at another visit often at a different setting.
The effects of treatment, if not immediately obvious, may be appraised at a later visit. Also, the progress of the disease is not predictable. It is necessary that at the end of a visit, the care provider use his/her discretion to plan what is to be done subsequently. Even so, the plan may have to be changed when the patient’s progress is reviewed at at the next visit.
Sequential Vs Simultaneous or Concurrent Procedures
Procedures, depending on their types, can occur sequentially or can be carried out concurrently. Two care providers may perform different procedures at the same time even in the presence of the patient. For example a doctor, may examine the patient while the nurse observes him/her. In joint-sessions, encounters with different care providers happens simultaneously. A good example is surgery and anesthesia. While they are working in tandem, each may be looking at different aspects and may want to arrive at their own findings and conclusions which may be documented separately. Otherwise, a joint statement may be recorded by the leader of the team. For example, surgical operation is a joint-session where the surgeon, anesthetist, and nurse conducts different procedures.
Encounters and non-encounter procedures can always happen concurrently. For example, laboratory tests on samples can be performed at the same time or a slightly later time as other procedures.
Duration Of Procedures
The duration of procedures cannot be predicted with certainty. For this reason the duration of visits is also uncertain. This is because:
- procedures are made up of processes that take a variable time to complete
- results takes a variable time to be made available
- resources for certain procedures are limited and shared such that access to them have to be scheduled.
Setting for Procedures
Just like the visit, procedures also are performed at special locations, date, time and assigned to particular persons to carry them out. Resources (room, machine, materials or person) are finite and often scarce. Procedures can take place only if the room, machine or care provider is free. Therefore at a visit, the procedures for various patients has to be scheduled or sequenced in queue. Knowing the type of procedures to be done, as indicated in the care plan, allows the care provider to schedule the procedures in advance.
For a visit, a patient is assigned to a particular service delivery unit. Each unit will have specific settings i.e. the facility design (layout) and the resources made available to enable various procedures to be carried out. Outpatient clinics, daycare units, inpatient wards and intensive care units will have different layouts and facilities. A typical outpatient clinic layout is depicted below:

Conversion of Reference Plan to Actual Plans
The reference SOP/Care plan is conceptual. The challenge therefore is to find the way to transform it into a plan that is practical taking into consideration the capabilities of the facility where it is to be implemented including its viability as a business venture. The Reference plan is not rewritten as a complete Actual document but the pertinent parts are conceived as and when planning becomes necessary at various points of care. The care provider has to go back and forth between reading the reference plan and actual planning. Hence the reference plan must be readily available. This reduces reliance on memory. When and how to perform routine and mundane tasks need not be spelt out but should follow common accepted practices.
Plans as Instructions
Plans are intentions that are executed through instructions which in practice are called orders. In the Reference Plan instructions or orders are laid out according to phases of care and proceed continuously as if in a contiguous manner. However in practice, orders can be be made in two ways
- scheduled before visits, or encounters, events)
- at the start or during sessions
Procedures or tasks are performed through made in during actual care based on those contained .In general, procedures are performed during visits. The exception is when the task has to be carried out by the patient at home (self care) or elsewhere in the interval between visits. The procedures to be done depends on the phase that the care is at.
Execution of Procedures
The conversion of the Reference plan to an Actual plan is the critical step in ensuring the success of the planning of clinical patient care. The SOP/Care Plan is thought of and written as a list of instructions. When executing the plan, the instructions are converted into orders. Orders are made more imperative than instructions by specifying:
- date and time
- method
- personnel responsible for performing it
- where it is to be done
The way the Actual plan is implemented depends on whether a traditional paper based system or a computerized system is used. Success depends on familiarity and awareness of care providers regarding both the Reference Plan and the Actual plan. For the Reference plan the care provider the important factor is availability and access. For the implementation of Actual plan, the key factor is communication and dissemination. Parts of the care plan can be made more easily accessible through the use of posters, booklets. protocols. In a computerized environment prompts, notification, alerts and links can be provided.
Orders, Tasks and Task Lists
Plans are executed as orders. Order sheets. Task Lists
Obtaining, Documenting and Viewing of Results,
Orders and tasks are managed differently in paper-based system as opposed to computerized systems. The subject will be discussed in detail in separate sections.
Execution of SOP/Care Plans
The Clinical Care Procedure is made up of tasks or processes. To initiate tasks, requests, instructions, or intentions are made. They are generically termed as ‘Orders’. Through them, a care provider declares his/her choice of plans and communicate to others involved in the care of the patient. The privilege to ‘order’ tasks depends on the role of the care provider. The primary provider (lead practitioner), usually a doctor or nurse practitioner, selects the general plan which would contain instructions and orders for all care providers involved. Specific care providers in the team may modify or add further orders pertaining to their area of care. Once made, orders become tasks to be performed. The tasks are listed and addressed one by one by the person responsible to perform them. Once completed, the task would have a result which can be in the form of:
- success (completion) or failure of performance
- the data generated as a result
From a financial perspective, each task can be given a charge which can be billed once the task is performed.
Use of SOP/Care Plans in Combination with Work Instructions
The most important link is to work instructions for performing common standard procedures (setting up machines, dilution of drugs etc) responses to incidents (cardiac arrest, respiratory failure, anaphylaxis, death etc.) or reference standards (drug dosages, regulations etc.).
MAPPING PHASES OF CARE TO SESSIONS
The logical sequence of phases is:
- establishing diagnosis, stabilization and immediate care
- initiation of care
- optimization of care
- maintenance (continuation) of care, re-evaluation and modification
- resolution of care based on resolution of illness
Conceiving the Actual Plan
The actual plan is not rewritten in total but are conceived as and when planning becomes necessary at various points of care. The care provider has to go back and forth between reading the reference plan and actual planning.

MAPPING PROCEDURES TO STEPS IN THE PLANNING PROCESS
The steps to be taken includes:
- Start by determining the working diagnosis
- Selecting the reference SOP/Care plan matching the working diagnosis
- using it as a guide to construct the actual plan
- dissemination among the care team
- ensuring conformance / adherence to it
- measuring the quality of the intermediate and the final product
- continually improving the processes and outcome
- putting in place remedial measures when necessary
MAPPING PROCEDURES TO SESSIONS
The advantage using Reference SOP/Care Plans in the care of patients is in
- Phase of care
- adherence to Sequence of the care processes
- determine which plan to choose
Sequence of Procedures within Various Phases Phases



Providing Care with the Aid of SOP-Care Plan
as Guide
- STEP 1: Match the the service product with the Needs of the Patient
- STEP 2: Be cognizant (aware) of Standards for the Expected or Desired Outcome to be achieved
- STEP 3: Ensure that the Service Delivery System is appropriate for the service product to be delivered
- STEP 4: Follow closely the Method of Delivery of the Service Product
Step 1: Match the the service product with the Needs of the Patient
Identification of the Service Product
Choice of the Appropriate Reference SOP/Care Plan
Matching Phases with Visits
Sequence of Phases in a Care Episode
n
- Phase of determining the diagnosis and immediate care / early treatment
- Phase of initiation of definitive care
- Phase of optimization of care
- Phase of maintenance of care
- Phase of resolution (continuation or discontinuation of care)
Sequence of Procedures within Various Phases Phases
Execution of Plans Plans in Paper-Based System
To construct the Actual plan, the provider need to read the relevant parts of the Reference plan, at the point when planning is required, transform it in his/her mind or jot it on a piece of paper before transcribing (rewriting) it onto the case notes (paper medical record) as instructions. Obviously, this is a laborious method and is the reason why attempts at using care plans (e.g. by nurses) have met with limited success. It works only if the care provider is very familiar with the plan to the extent he/she has it in memory and can construct the actual plan on the go.
In a paper-based system, the plan takes the form of instructions documented in the medical record regarding tasks to be performed for all aspects of care including investigations, monitoring, and various types of treatment such as nursing care, medication, procedures, rehabilitation, counseling, psycho-social aid etc.
Traditionally, the actual plan is documented as shown below:
Planning is considered as a distinct and separate task. Data concerning it, is recorded at the time when the plan is generated together with other related tasks in chronological order.
Currently, there is a practice of using a separate table to record the plan together with assessment, tasks performed and outcome achieved, in the case notes. Putting these together in one table is incorrect because those activities occur at different time periods.
Plans are executed as orders written in the medical record. The orders are then rewritten on Order sheets which are passed to the relevant unit or person who is supposed to carry them out. Results are returned on result sheets which are appended to the main record. Monitoring data is recorded on separate charts which are compiled together with compiled with the main records at discharge. The practice of writing Nursing notes on separate charts should not be condoned.
Instead, the execution of the plan (the tasks done), and the results obtained are documented, as and when the processes are performed, in progress review notes, monitoring charts, procedure records, findings, outcome documentation and etc.
Execution of Plans Plans in Computerized System
Using SOP/Care Plans as a Guide to the Practice of Clinical Patient care
- Start by determining the working diagnosis
- Selecting the reference SOP/Care plan matching the working diagnosis
- using it as a guide to construct the actual plan
- dissemination among the care team
- ensuring conformance / adherence to it
- measuring the quality of the intermediate and the final product
- continually improving the processes and outcome
- putting in place remedial measures when necessary
Maximizing Benefits of SOP/Care Plans through the Use of Computerized Systems
While computerization is conducive for implementing SOPs/Care Plans, the system itself is best designed based on them. The benefits are complimentary.
Making SOP/Care Plans as Basis for Designing Computerized Clinical Information System
- what the clinician intends to do
- the information required for performing it
Use of Information by the Clinician
Clinical care activities is a series of data management activities, which include:
- Data collection (gathering, capture, input, entry)
- Data storage (accumulate and make available)
- Data extraction (retrieval, output)
- Data transmission (submission, retrieval)
- Data analysis and interpretation (use)
- Data presentation (display, view)
The User-System Interface
The user interface of the Clinical Information system has two main functions:
- Provide information
- Facilitate work
Provision of Information
The system provides two types of information
- Data regarding the case obtained during the course of work
- Reference information
Depending on needs, the data can be from the current episode, the previous visits or the current visit. All activities (tasks performed and events that happen) will generate data which will be stored in the database.
Reference information is the information prepared and endorsed by the facility for use by the users within it. They are stored in a file server and made available as read only documents.
Viewing Existing Data
Only via EMR
- the previous visit in the case of an outpatient case
- the last few days of the current visit in an inpatient case
- the current week or month or defined by dates
- the entire visit
- all visits is the current episode
- other previous episodes
At the beginning of a session the clinician must be aware of the current stage of the flow of the clinical care process he/she is at. The stage of the process determines the amount data already available. Even in a new case, useful data is already available to the clinician.
At the start of a new case, the data displayed is limited to data regarding identification (gathered through Registration), the reason for visit and the care episode. However, in a referred case, a scanned image of the referral letter can be shown. If a questionnaire is given to the patient before hand, the replies can be made available.
In a case where the care has progressed, much more data resulting from what has already transpired is available. The data captured by an earlier care provider is always available to the subsequent provider. The data can be raw or analyzed and be presented in various format (spreadsheet view, lists, tables, graphs). By viewing it, the clinician is aware of what processes have been completed and what is to be performed next.
Presentation of Data as Means of Communication
Indicating What Has Been Done
- providing the necessary information
- anticipating what data to be gathered
- indicating what tasks are to be done
Providing Reference Information
The system should also supply the Reference SOP/Care Plan, information on standards such as lists of services, diagnoses, tests, drugs, surgical procedures and others.
Facilitating Work through Access to Reference Information
The most valuable reference information is the Reference Plan. At the start of his/her work, the clinician chooses a Reference care plan which is then modified to form the Actual pan. When the plan is executed, the choice of data gathering tools (forms), investigations, monitoring methods and treatment is built in as part of the design
- Work Instructions
Before starting a consultation or encounter, the clinician must first of all know what has transpired before by viewing existing data. He/she will then be able to anticipate what further data needs to be acquired.
Data gathering (often termed as clinical documentation) itself is a very important part of the clinical care process. For identifying symptoms and eliciting signs or observing them, the system assists by providing the data gathering forms that will guide the clinician on the relevant areas to focus on. The collection of some data can be made mandatory. The forms can be designed such that a certain finding will lead to the necessity to gather more elaborate data regarding it. Data is also obtained by performing tests. This requires the placing and activating of orders in the form of order sets.
Toggle Between Provision of Information and Facilitating the Performance of Work
- a primary the menu including both on the same screen page or
- use of a toggle mechanism, that switches from one option to the other.
- the pertinent accumulated data to be viewed
- view the steps of the actual plan plan or the reference plan
Menu for the View of Existing Information
Menu for Facilitating Work Performance
Tasks (procedures) to be performed performance is provided as a menu listed below:
- Assessment
- Diagnosis Formulation
- Plan of Care
- Intervention
- Evaluation
- Case Disposal
Method of Using SOP/Care Plans in a Computerized System
Getting onto the Right Path: Choosing the Suitable Reference SOP/Care Plans
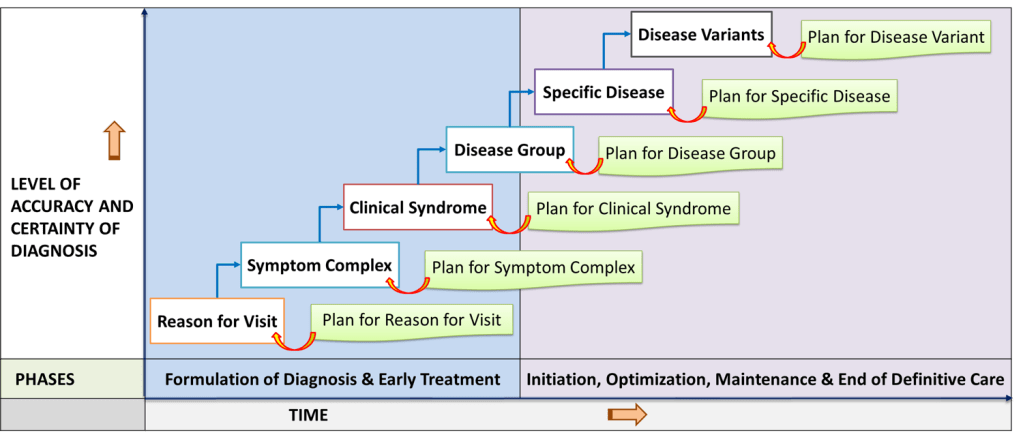
Diagnosis as the Defining Factor of the Service Product
SOP/Care Plans are designed for service products. In patient care the nature of the product is often unclear at first. Hence the initial service may be generic in nature i.e., applicable to a patient group rather than a specific type of patient. Later as the needs of the patient is clearer more specific plans are used. Even then, the Reference is still generic in the sense that it is applicable to typical patients with a typical disease condition (rather than an individual patient). After they are retrieved they will be modified by the care provider to formulate the Actual plan specific for the patient.
In the clinical process workflow, planning of care comes after the formulation of diagnosis. Changes in the diagnosis is documented by the care provider. He/she may then select the appropriate care plan for the latest working diagnosis. Alternatively, a more sophisticated Clinical Information System can be designed to put forward choices of plans. Once a plan is chosen, it can be modified based on analysis of the accumulated data. The clinician or automatically the system itself can make alterations to the plan e.g. perform a reconciliation by omitting redundancies.
- reason for visit
- symptom complexes
- clinical syndromes
- specific diseases
- variants of the disease
Making Available a Comprehensive List of Reference SOP/Care Plans
Standardized operating procedures or care plans of the healthcare facility should be made available for reference as a properly indexed comprehensive library of documents. The Reference plan for a particular case is selected from this library.
Library of Care Plans
Indexing of Care Plans within the Library
The Library of SOP/Care plan is arranged as folders indexed according to levels.
- Level 1 – the Diagnosis
- Level 2 – Phase of Care
Providing Plans According to Phases of Care on Just-in-Time Basis
System for Storage and Retrieval of Reference Plans
Reference plans can be made available as a library or repository accessible via a file server. The plans are read-only files that can be requested by users or can be automatically loaded when the situation demands. The basic structure of the system as shown below is incorporated into the Clinical Information System and accessed through it.
Choice and Selection of Plans. SOP/Care Plans can be designed to contain instructions which take the form of orders executable via the Order Management System (CPOE).
Menu for Selecting a Care Plan
Planning of patient care follow a two step process i.e.
- choosing an appropriate plan as a guide (termed as the Reference plan)
- Using it to create the plan which will be used in the actual care of the patient (termed as the Actual plan).
The menu for performing tasks will present some or all the clinical care procedures that the clinician intends to perform. These include:
Execution of SOP/Care Plans
The Clinical Care Procedure is made up of tasks or processes. To initiate tasks, requests, instructions, or intentions are made. They are generically termed as ‘Orders’. Through them, a care provider declares his/her choice of plans and communicate to others involved in the care of the patient. The privilege to ‘order’ tasks depends on the role of the care provider. The primary provider (lead practitioner), usually a doctor or nurse practitioner, selects the general plan which would contain instructions and orders for all care providers involved. Specific care providers in the team may modify or add further orders pertaining to their area of care. Once made, orders become tasks to be performed. The tasks are listed and addressed one by one by the person responsible to perform them. Once completed, the task would have a result which can be in the form of:
- success (completion) or failure of performance
- the data generated as a result
From a financial perspective, each task can be given a charge which can be billed once the task is performed.
Performing Clinical Care Processes
Menu for Executing the Plan (Performing Tasks)
The sequence of items in the menu follows the general convention of the clinical care process adhered to universally by clinicians (roughly as listed below).
- Assessment
- Subjective
- Objective
- Diagnosis
- Planning
- Order Set
- Intervention
- Task lists
- Evaluation
- Observation
- Monitoring
- Reassessment
- Progress Review
- Outcome assessment
- Case Disposal
- Review of Plan
The content may be some or all of these depending on the situation i.e. the type of visit, the phases of care and completion of tasks.
The Critical Role of the Order Management System
The support systems perform tasks which can be the performance of tests or supply of items as requested.
Specific Plans to be Made Available in the Library
- reason for visit
- symptom complexes
- clinical syndromes
- specific diseases
- variants of the disease